Real life: ‘I beat high cholesterol without pills’
Peter Gordon didn't want to take statins, so he turned to natural remedies. Here's how he did it
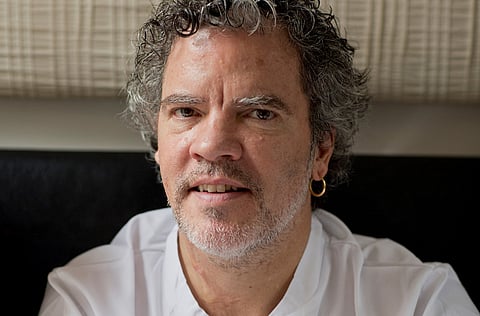
He runs four top restaurants on two continents, yet chef Peter Gordon still finds it hard to walk past a Kit Kat. Add cakes, doughnuts and biscuits to his known foodie weaknesses, along with fatty meats and it’s no surprise that, four years ago, Gordon was diagnosed with high cholesterol and prescribed statins. However, while doctors were predicting a heart attack, he opted to use diet and exercise instead of taking the pills. Today, Gordon is not only 6kg lighter, his cholesterol has dropped.
“I’d had a slightly raised cholesterol of around 6.8 since about 2008 but in 2012 it jumped to 8,” Gordon, 53, explains over Skype from Auckland, where he was born and now runs the Sugar Club restaurant and Bellota.
Gordon — whose eighth cookbook is out this week — splits his time between New Zealand, where his partner Al, CEO of a law firm, is based, and London, where he runs The Providores and Tapa Room in Marylebone and Kopapa, a café-restaurant in Covent Garden.
Sweet, fatty food
A fan of fresh, healthy produce, Gordon also loved things sweet, fatty and rich. “I would look at an almond croissant and think ‘I need to eat that, I need to eat potatoes roasted in duck fat.’ There’s temptation on every plate and of course, I have to taste everything.”
When his doctor recommended a statin, Gordon was reluctant. “Everything I had read seemed to imply statins had long-term effects — if there was a more natural way, I wanted to try it.” With a staggering 65 million prescriptions written for cholesterol-lowering statin medications last year, they are now the most prescribed drug in the UK. Data for the UAE is unavailable.
Yet one study from February 2015 found that the benefits of statins had been exaggerated and a significant number of patients — including Gordon — are wary, says Dr Imran Rafi, a GP and spokesman for the Royal College of General Practitioners.
Side effects
“Statins can cause inflammation in the liver,” he explains. However, Dr Rafi admits it is rare, and adds: “I can’t think of the last time I had to take someone off a statin because their liver had become upset.”
Once you come off statins, liver effects are reversed, but other common side effects include muscle aches and pains (the key reason people stop taking them) and increased risk of diabetes, nosebleeds, headaches and sore throats and, less commonly, inflammation of the pancreas, dizziness and acne.
Until he asked, Gordon had no idea a number of his close family also had high cholesterol. “After the diagnosis, I spoke to my family and my mother, three sisters and dad all have high cholesterol, but there are no heart attacks in the family. I thought, ‘if we’ve never had a heart attack death in the family, I have low blood pressure and I don’t smoke, why take statins?’”
Family threat
Peter Weissberg, Medical Director of the British Heart Foundation (BHF), says most of us will inherit some elements of our cholesterol from our family, but Gordon’s instincts were right: no single risk factor should be treated in isolation. “High cholesterol alone — in someone who doesn’t have high blood pressure, doesn’t smoke [or] have a family history of premature deaths from heart attack — isn’t as bad as if [they] had any of those or all of those risk factors, along with the high cholesterol.”
After consulting a practitioner of Kampo — Japanese natural medicine — about ways to lower cholesterol, he was told to increase his intake of soya foods such as tofu, soya milk and soya sauce, and to take a supplement called red yeast rice. “It’s a type of bacterial fungus I had cooked with before and knew it was something the Chinese threw into fatty pork dishes with the belief that it offset the cholesterol in the food. It sounded like hocus-pocus but I looked into it and found it contained a natural statin.”
Gordon also increased his intake of psyllium husks, a natural soluble fibre. The beloved biscuits and sweets were replaced by spelt crackers and hummus with vegetables, which he could snack on after a late evening working, and fatty meats substituted with lean steaks. While the effectiveness of red yeast rice is still being debated, the other changes Gordon made are well-proven, according to Tracy Parker, Chief Dietician at the BHF: “Lowering intake of fat from meats, cakes and biscuits and increasing cholesterol-lowering foods such as vegetables and soya bean products can help lower LDL [bad] cholesterol by up to 24 per cent, so he is on the right track.”
Though he hates the gym, Gordon has loved swimming since he was a young boy. “I started swimming two to four times a week for half an hour — in the harbour when in Auckland or Olympic pool in Stratford when in London.” He also began walking to the Tube station and stepping up the escalators when he could. “I’m busy, I’m often jet-lagged, I’m not the person that can go to the gym every day, but this way I can fit exercise in and I feel more virtuous for it.”
The proof
In December, Gordon had his last cholesterol reading. “My total cholesterol was 6.8 so it had dropped an entire point and within that my good cholesterol had increased from 0.9 to 1 and is now in the healthy range and my bad cholesterol had decreased from 5.8 to 4.7. It’s still not the level my medical professionals want, which is an overall cholesterol of around 5.0, with bad cholesterol around 3.0, but it’s a marked change.
“I feel more vibrant now and I think that’s a combination of the weight loss and being more aware of what and how much I am eating.”
— The Daily Telegraph/ The writer is editor of Healthista.com


