Coronavirus mutation: What virologists found
Mutated SARS-CoV-2 a big boost for infectiousness as experts debate its deadliness
Highlights
- There's a new SARS-CoV-2 variant carrying a change (mutation) in the spike (S) protein.
- This viral spike amino acid change, known as G614, has made it the most prevalent strain in the global pandemic.
- Virologists who conduct real-time tracking of viral mutations found a recurrent pattern of G614 increasing in different parts of the world.
- The strain makes the virus more infectious (higher “viral shedding” capability).
- It’s too early to say whether the strain would end up being deadlier — or less potent.
Dubai: Viruses are interesting creatures. They are neither dead nor alive. They occupy that grey area between living and non-living things. Yet they cause such devastation.
In reality, viruses are complicated assemblies of molecules — proteins, nucleic acids, lipids, carbohydrates.
Here's the freaky part: They DO NOT multiply on their own. They need a host to reproduce.
They need us (living host cells in humans, animals or plants) to spread their genes as they do contain genetic information — and are therefore subject to evolution and natural selection.
Like living cretins, viruses mutate too.
Now think about this: A virus that kills everyone is also dead. Evolutionary biologists say that a virus strain that kills a host instantly would eventually fizzle out over time — a dead host cannot pass on the viral genetic information to another host.
This is because a virus' ultimate reason for being is to live, pass on its progeny, by constantly replicating and not killing all potential hosts.
Genetic mutation
To do this, it must adapt. Change into something else, even if in minute parts.
And that's what scientists see. Recently-published studies show virologists have seen tiny genetic mutations in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19.
As it infects more people across the world, experts are also tracking its spread and evolution — in real time — to bump up our knowledge about it, and guide health authorities on control measures.
How do scientists track viral mutations?
Here’s one: A virus behaves a bit like the game of “telephone”. As the whispered sentence is passed from one person to the next, it changes slightly.
Data on SARS-CoV-2 show that it mutates an average of 2 mutations per month.
How do we know this? Scientists all over the world are collecting samples from patients with COVID-19, sequencing the virus’ genetic code, and uploading them on to a scientific server, called GISAID.
Overall, evolutionary rate for SARS-CoV-2 is "very low", say experts.
But they also found something more: As the virus travels within and between countries, it mutates — a reaction to evolutionary pressure from the population it “invades”.
Given this tiny mutation and its implications for the current pandemic, scientists must anwer two vital questions on this novel coronavirus:
Is SARS-CoV-2 getting more infectious?
Yes, say several studies. One, published on July 13, 2020 in NEJM Journal Watch (as a pre-print), showed that mutated coronavirus have demonstrated a significant “boost in infectivity”.
Researchers using time-lapse and viral sequences analysed from 999 patients hospitalised with COVID-19 found something interesting: in 30 out of 31 regions of the world, a virus strain known as “D614” was dominant initially.
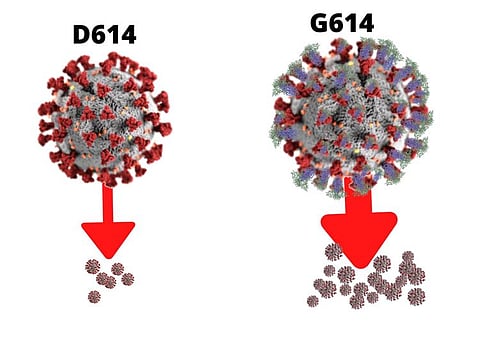
Over time over, however, the strain “G614” (known to scientists as just the “G” strain) took over.
How and why did this mutation happen?
How the strain moved from D614 to G614 remains a mystery.
But scientists said it’s an “asynchronous” transition — which increasingly occurred in different regions throughout the world.
It generally started in Europe, followed by North America and Oceania, then Asia, researchers found.
GISAID MUTATION DATABASE
Each day, hundreds of new SARS-CoV-2 genetic sequences are added to GISAID. Data uploaded by virologists from around the world on GISAID (Global Initiative for Sharing All Influenza Data) show the dominance of the G strain. Of the approximately 50,000 genomes of the new virus that researchers worldwide have uploaded to the GISAID database shared by the world’s virologists, about 70 percent carry the mutation — officially designated D614G but known more familiarly to scientists as “G.” GISAID sequences are generally linked to the location and date of sampling. Based on a May 29, 2020 download of the GISAID data, (when the Spike alignment included 28,576 sequences); updated versions of key figures can recreated on the website (cov.lanl.gov).
Another important bit: Scientists found that the “cycle threshold” (Ct, a measure of PCR test) was lower in the G strain.
This indicates a higher “viral load” (the lower Ct, the higher the infectiousness). It simply means the G strain is more infectious.
Higher viral titers (concentration of antibodies in blood) were also seen in samples with the G614 variant than with the D614 variant.
Different research teams sought to identify mutations in the SARS-CoV-2 spike protein, which they believe is an important factor for its infectiousness.
MUTATION IN AMINO ACID 614
There are about 1,300 amino acids that serve as building blocks for the Spike protein (exo-protein) on the SARS-CoV-2 viral surface which gives it like a crown-like profile. In the mutant virus, the genetic instructions for just one of those amino acids — number 614 — switched from a “D” (short for aspartic acid) variant to a “G” (short for glycine).
Why is the Spike protein important for the coronavirus?
The spike protein is the “key”. It allows the coronavirus to enter human cells efficiently, in a sort of lock-and-key mechanism.
A team from Scripps Research had confirmed this “infectivity boost” in another study.
But here’s the interesting bit: While the mutation increases infectivity, it reduces “shedding”. Shedding is virology-speak for the expulsion and release of virus progeny (produced in the host, like a COVID-19 patient) following rapid reproduction.
In another study, published in PNAS (Proceedings of the National Academy of Sciences), researchers at the University of Minnesota (UM) identified the biochemical mechanism that may explain how the virus infects people efficiently — while evading their immune responses.
This study, led by Prof Fang Li, of the University of Minnesota College of Veterinary Medicine, examined the mechanism by which SARS-CoV-2 enters cells.
Specifically, the team investigated how the virus "unlocks" human cells using a surface “spike” protein as the "key."
What Dr Fang's team found:The tip of the viral key binds strongly to human cells. They also found that tip of the viral key is often “hidden”. Moreover, when new virus particles are made, the viral key is already pre-activated by a human enzyme.
Similar findings were found by a team from Los Alamos and Duke in the US and Sheffield Teaching Hospitals in the UK.
The US-British team identified at least 14 mutations in the spike protein, but highlighted that the mutation spike D614G is of "urgent concern”.
They found that the strain began spreading in Europe in early February. When introduced to new regions, it rapidly became the dominant form.
What were the key findings of these studies?
Is the virus progressively becoming harmless?
That's the hope.
And there’s an expectation that, unlike in the movies where the virus gains higher infectiousness and deadliness, viruses in real life progressively become "harmless" as its relative viruses responsible for the common cold, for example.
But this is not to say they are indeed harmless now. Mutations take time.
What is RT PCR cycle threshold (ct)
In a real-time polymerase chain reaction (PCR) assay, a positive reaction is detected by accumulation of a fluorescent signal. The Ct (cycle threshold) is defined as the number of cycles required for the fluorescent signal to cross the threshold (ie exceeds background level). Ct levels are inversely proportional to the amount of target nucleic acid in the sample (ie the lower the Ct level the greater the amount of target nucleic acid in the sample). Cts < 29 are strong positive reactions indicative of abundant target nucleic acid in the sample Cts of 30-37 are positive reactions indicative of moderate amounts of target nucleic acid Cts of 38-40 are weak reactions indicative of minimal amounts of target nucleic acid which could represent an infection state or environmental contamination.
Why do viruses lose potency over time?
Prof Fang explains: “Typically when a virus develops mechanisms to evade immune responses, it loses its potency to infect people.”
But is the coronavirus totally harmless now?
No. When asked about comments made by the Italian doctor (i.e. that the coronavirus is losing potency and has become less lethal), a WHO expert issued a warning instead.
Right now, the coronavirus is NOT losing its potency, said Dr. Mike Ryan, executive director of the WHO’s emergencies program.
"LESS AGGRESSIVE" VIRUS? ITALIAN DOCTOR EXPLAINS
Dr. Massimo Clementi, director of the microbiology and virology laboratory at San Raffaele Hospital in Milan, explained why viral potency eventually goes. He gave this illustration: During the peak of deadly infections, between the end of March and the first half of April, up to 80 people were arriving sick every day at San Raffaele Hospital. He said: “Most of them were admitted immediately to the intensive care unit (ICU), and very often, we couldn’t save them." But in recent weeks, he pointed out, things have changed a lot. "Our ICU isn’t under pressure anymore and we even have more beds available. A scenario like this was unthinkable for us in the peak of the infection.” He said that based an evaluation of the clinical expression of the infection, shows the virus “now less aggressive”. Dr Clementi said new viruses are always “very aggressive” in the first phase, “then they learn to live with their victims, allowing them to survive. If a virus kills, it can’t replicate.”
“We need to be exceptionally careful that we are not creating a sense that, all of a sudden, the virus has decided to be less pathogenic. That is not the case at all,” Dr Ryan said.
TAKEAWAYS
• Scientists say SARS-CoV-2 is not highly “mutable”, meaning that it does not mutate or transform fast.
• Data published in the New England Journal of Medicine (NEJM), however, show that coronavirus variants may arise relatively “quickly”.
• Most scientists believe that even though this variant appears to be more infectious (spreads faster, as evidenced by its lower RT PCR Ct) it did not appear to be more virulent.
• In limited lab tests to measure viral quantity and reactivity using assays, researchers found the variant was still inactivated by convalescent sera.
• This means that T-cells taken from the blood of people who recovered from COVID-19 were able to neutralise the G visual strain.
• If we do not wear masks properly, do not social distance or observe basic hygiene measures (washing hands properly), the virus will get to us.
• If we let the virus go, it will transmit, infect more people and will still cause severe illness in some people.
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox









