Dubai: Remdesivir is still considered an experimental antiviral, patented in the US, with another patent application in China. Its US licence is under the "emergency use" case on coronavirus patients.
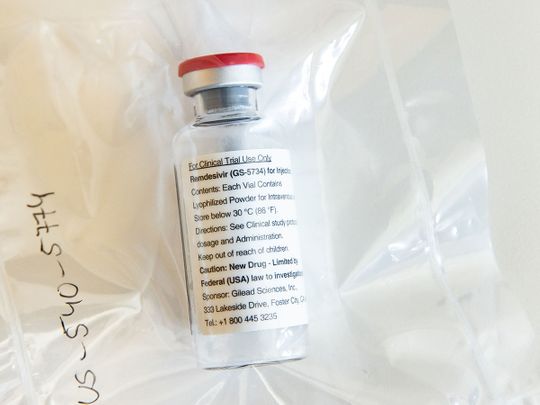
Developed by US biotech firm Gilead Sciences, remdesivir was first patented in 2017, back when the company was originally targeting it as a possible treatment for the Ebola virus, which first broke out in 2013-14.
In trials, remdesivir was seen to help reduce death rates down to 33 per cent among Ebola patients — if victims received the treatment early enough after becoming sick when viral loads were still now, according to a Wired report in December 2019.
At least three other Ebola treatments, however, were reportedly proven to work better in reducing fatalities, compared to remdesivir following trials in Africa. These are: ZMapp (by Mapp Biopharmaceutical Inc), mAb114 (by the US National Institute of Allergy and Infectious Diseases, NIAID), and Regeneron's REGN-EB3, according to the Wired report.
But due to biochemical similarities in how the Ebola and SARS-CoV-2 viruses function, Gilead had seen an opportunity to "repurpose" remdesivir to treat COVID-19 early in 2020.
A study published in January 2020 in the New England Journal of Medicine reported that a US coronavirus patient was found to show an improvement after taking remdesivir.
The SARS-CoV-2 virus, however, acts sort of the same way using a spiky protein that easily binds to ACE2 (angiotensin-converting enzyme 2), the receptor protein of both SARS-CoV and SARS-CoV-2, which is abundantly present human lung epithelial cells and small intestine. The virus clobbers the lungs.
What is the fair price for remdesivir?
In 2018, The Lancet published a study estimating the cost of developing at least one vaccine through to the end of phase 2a for each of the 11 epidemic infectious diseases at a minimum of $2.8 billion to $3.7 billion (or somewhere between the $1.2 billion to $8.4 billion range).
The Institute for Clinical and Economic Review (ICER) — a Massachusetts non-profit research outfit which studies drug development costs — says remdisivir is cost-effective at $4,460 per course of treatment.
$ 4,460
The Institute for Clinical and Economic Review (ICER) — a Boston-based non-profit that studies drug costs — says the drug is cost-effective at $4,460 per course of treatment.Gilead, based in California, is now ramping up supply with the aim to treat 1 million patients by the end of the year, according to one report.
This month, Beximco Pharmaceuticals, one of Bangladesh's largest drugmakers, will start remdesivir production under Gilead licence, a senior company executive stated.
A Reuters report on Wednesday (May 5, 2020), states that the company plans to price the drug, administered via intravenous infusion, at between $59-$71/per vial, according to Beximco's Chief Operating Officer Rabbur Reza, adding a patient might need anywhere between 5 and 11 vials.
There are claims on social media that since the drug was developed using US taxpayers' money, and it costs only $10 (about Dh37.50) per vial to manufacture — this claim cannot be immediately verified — the emergency COVID-19 vaccine should then be priced much less.
Vaccine patents
Gilead's remdesivir patents mean that it has a monopoly on the drug in the US. Barring government action or Gilead licensing the patent to others, it's the only company that can manufacture it.
Gilead's patent expires in 2037, at which point a generic version could be possible.
On February 4, 2020, Reuters reported that the Wuhan Institute of Virology (WIV) had applied for a patent on the use of Gilead's remdesivir in China.
The application was submitted jointly with China's Military Medicine Institute of the People’s Liberation Army Academy of Military Science, according to the Wuhan Institute of Virology.
That was the same day Cell Research published the results of a clinical study in China showing remdesivir and chloroquine, together, "effectively inhibited" the SARS-CoV-2 (then called 2019-nCoV) in vitro.
One of the authors of that study was Prof Shi Zhengli, also known as the Chinese "bat woman" credited for her extensive research on bat coronaviruses, including WIV studies funded by the US government.
On May 2, 2020, US authorities approved remdesivir for emergency use on coronavirus patients, as more US states eased lockdowns despite another spike in deaths from the disease.
The US approval is the latest step in a global push to find viable treatments and a vaccine for the coronavirus, which infected more than 3.3 million people.
Parallel vaccine research: Racing against the clock
Dozens of research are currently being undertaken to find the treatment or therapy against SARS-CoV-2 that works and is safe.
Strategies include screening for the best way to neutralise the SARS-CoV-2 spike proteins that make them easily bind to human cells in the lungs and intestines, or activate the antibodies that did the best job of binding to the spike proteins of SARS-CoV-2, or both.
The UAE is also leading a pioneering stem cell-based therapy to help cure COVID-19 patients.
Unlike the vaccine route, the revolutionary stem cell-based therapy developed by a UAE team acts by repairing lung damage through an inhaler sourced from activated stem cells harvested from patients themselves.
The US licence of Remdesivir, administered intravenously, is under the "emergency use" case on coronavirus patients.
The development of such drugs, however, is a notoriously slow process, as it takes many years of painstaking reverse-engineering work.
For example, Zmapp was developed by infecting mice with Ebola and then collecting the antibodies the mice produced against the virus. The, those antibodies had to be further engineered to look more like a human antibody, so as not to provoke an immune reaction.
The trials also takes many months, if not years, to confirm if the treatment is safe and effective.








