Why some people get many types of cancers; genes, earlier treatments, DNA alteration
Data shows that common inherited factors, treatment can influence risk of second cancer
Noelle Johnson, 42, was diagnosed with her first cancer — a soft tissue sarcoma under her right arm — in 1999 when she was 21. In 2013, her physicians found six different cancers in her breasts. In the years that followed, surgeons discovered and removed numerous masses they deemed “premalignant” from her ovary, her uterus, her leg, arm and chest wall, aiming to get them out before they turned cancerous.
Each tumour was distinct, that is, none resulted from the spread of any of the others. For Johnson, having multiple primary tumours diagnosed at an unusually young age was both scary and baffling. “It was crazy,” recalls Johnson, who lives in Windsor, Colorado, where she operates a day-care centre in her home. “My world started to spin. It was a huge red flag.”
Many people assume that when cancer shows up following an earlier tumour, it is a metastasis from the first. But this is not always the case. Multiple primary cancers can arise by themselves, and researchers in recent years have begun to unravel some of the reasons.
“Cancer therapies have improved dramatically in the modern era, resulting in a growing population of cancer survivors — over 15 million,” says Stephen J. Chanock, director of the division of cancer epidemiology and genetics at the National Cancer Institute (NCI). “As these individuals live longer lives, some of them go on to develop second cancers, tumours unrelated to their original cancer. There likely are multiple factors involved, and we are still learning about their causes.”
Treatment leading to more?
Experts believe that many of these additional primary tumours are the result of earlier treatments for initial cancers that often occur in childhood. Radiation and chemotherapy, while successful in knocking out the first disease, also cause DNA damage. This can prompt new cancers to develop later, among them lymphomas, leukaemia, and those of the breast, thyroid or soft tissues.
Other factors that can encourage new tumours probably include environmental exposures, such as tobacco or alcohol use, hormonal influences, viral infections — especially HIV — and genetics, which appears to be a major player. Also, experts believe that a combination of these is involved. “There are emerging data that suggest common inherited factors together with treatment can influence the risk of developing a second cancer,” Chanock says.
Finally, there also is the element of chance — somebody has to be first — that is, a spontaneous gene mutation that ultimately is passed on, beginning the chain.
Born with a cancer prone gene
Johnson wondered why she was susceptible to so many cancers. Six years ago, she finally found out: genes.
In 2013, after undergoing a double mastectomy — and before the later masses were found — genetic testing showed she had Li-Fraumeni Syndrome (LFS), an inherited familial predisposition to a wide range of specific and often rare cancers, particularly in children and young adults.
These often include breast cancer, osteosarcoma — a form of bone cancer — and cancers of the soft tissues, brain tumours, leukaemia, and a cancer called adrenocortical carcinoma that affects the outer layer of the adrenal glands, according to the National Institutes of Health. One parent with the mutation is enough to pass it on.
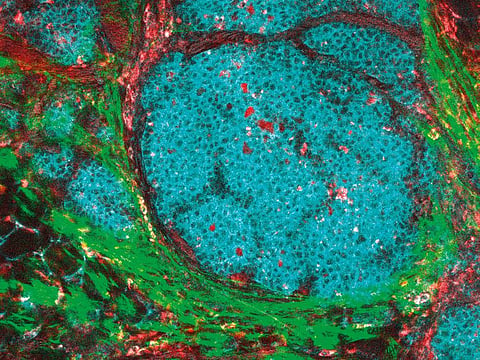
LFS involves inherited mutations in the TP53 gene (and also sometimes — but less often — the CHEK2 gene), a tumour suppressor gene which, undamaged, controls the spread of cancerous cells. When mutations occur, cells can divide, proliferate and form tumours. Other genetic and environmental factors also probably enhance the cancer risk in those with TP53 mutations, according to NIH. The cancer institute has a study under way trying to learn more about the syndrome.
It is unknown how many carry these mutations, although the Li-Fraumeni Syndrome Association reports that more than 1,000 multigenerational families worldwide have it. Researchers think it’s a conservative estimate.
“Historically, LFS is thought to be very rare,” says Kim Nichols, who leads the cancer predisposition group at St Jude Children’s Research Hospital in Memphis. “The medical literature says between 400 and 500 reported cases, but I truly believe there are more. Everyone hasn’t been diagnosed because it isn’t on most oncologists’ radar screens. For me, it’s very obvious, but in the real world, where oncologists treat many cancers, they don’t always think of it.”
The failure of many physicians to take a family history is one reason it is underreported, she adds. Cancers among closely related family members — especially at a young age — are an important clue. Johnson’s mother, for example, who died at 50, suffered from leiomyosarcoma, an aggressive cancer of the smooth muscle tissue. “Doctors often don’t think about the possibility of an underlying genetic predisposition,” Nichols says.
She and others point out that other genetic variants can result in multiple tumours, including those in the BRCA1 and BRCA2 genes, known for causing breast and ovarian cancers in women, but also are linked to such malignancies as pancreatic and prostate cancer, melanoma — including in men — and male breast cancer. Also, variants in the DICER1 gene can predispose individuals to many types of tumours, both malignant and benign.
Rb1 gene
Retinoblastoma, a cancer of the tissues in the retina that typically afflicts children younger than 5, can be hereditary or sporadic, but survivors with mutations in the Rb1 gene can later develop sarcomas, melanoma, and cancers of the brain and nasal cavity. Radiotherapy used to cure retinoblastoma appears to raise the risk, suggesting a possible interaction.
Moreover, researchers believe there could be numerous common genetic variants involved in the development of multiple tumours, as yet unidentified.
“It’s not just rare variants that we should be thinking about with multiple cancers, but common variants, possibly many of them,” says Lindsay Morton, a scientist in NCI’s division of cancer epidemiology and genetics.
Morton’s research focuses on treatment-related second cancers, including the interaction of genetics with the effects of the earlier therapy.
“This is a different way to think about precision medicine,” she says. “Usually people are thinking about targeted therapy, but we’re saying that the risk/benefit assessment for a certain treatment could depend on someone’s genetics. It may be that individuals have a genetic variant that reduces the ability of their normal cells to repair DNA damage from the cancer treatment, compared with someone else who doesn’t have that genetic variant.”
Nichols agrees.
“We know that when individuals are treated for first cancers, many of the drugs or radiotherapy kills the cancer cells by interfering with the DNA,” says Nichols, who is an investigator in NIH’s Li-Fraumeni study and a collaborator in a multi-institution LFS research consortium. “When that happens, you can introduce a change in the DNA that can lead to cancers down the road. The question is: How much of a risk came from treatment, and how much from an underlying genetic condition? We are learning about that now. It hasn’t been comprehensively studied, and it needs to be.”
LFS? Cancer can't be prevented
With LFS, there is no way to prevent the cancers. Experts believe the best way to cope is to detect and treat them early.
Joshua Schiffman, professor of paediatric hematology/oncology at the University of Utah’s Huntsman Cancer Institute and medical director of the Family Cancer Assessment Clinic, has been studying LFS for more than 10 years. He got involved after treating a 4-year-old with leukaemia who earlier had suffered a brain tumour. When examining family history, Schiffman found the child’s father and uncle both had died of glioblastoma, an aggressive brain cancer.
“We knew there must be something going on,” Schiffman says. “We tested her and her siblings, and discovered this was a family with LFS.”
He is researching the genetics of LFS by studying elephants, who seldom develop cancer. Elephants have 40 copies of the TP53 gene, compared with humans, who only have two. “We are trying to understand the molecular basis of how elephant TP53 functions, and how it differs from human TP53,” Schiffman says.
Meanwhile, Schiffman believes in using a whole-body MRI to detect tumours early, and has collaborated in several studies that suggest the approach works. The first, in 2011, led by David Malkin of Sick Kids Hospital in Toronto, followed a small group of LFS patients for five years, some of whom opted for screening, while others did not. After five years, those who elected imaging were still alive, compared with only 20 per cent who refused.
The regimen, known as the Toronto Protocol, is recommended by the National Comprehensive Cancer Network. But imaging is expensive — Schiffman estimates it costs from $3,000 to $10,000 — and he says many insurance companies won’t cover it. A recent study he wrote demonstrates it is cost-effective compared with treating cancer found later. “We know there are hundreds of patients who may have cancer growing inside them, but can’t afford the scans,” he says.
Johnson’s family —she has four sons, two of them LFS positive — are part of the NIH study. She expects more cancers are coming, “but we are working to find them early and remove them,” she says.
Meanwhile, she says she tries to keep anxiety in the background.
“Time is a gift, not a guarantee,” she says. “I’m a firm believer that our days are numbered. But our quality of life is still within our control.”
–Washington Post
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox



