Six top reasons to be optimistic about Covid-19
Among all the bad news around coronavirus, there is a silver lining too
Also In This Package
To help get through the coronavirus storm (and all the bad news), we must keep track of positive developments, too.
Here are six positive developments to remind us that there is hope in this crisis:
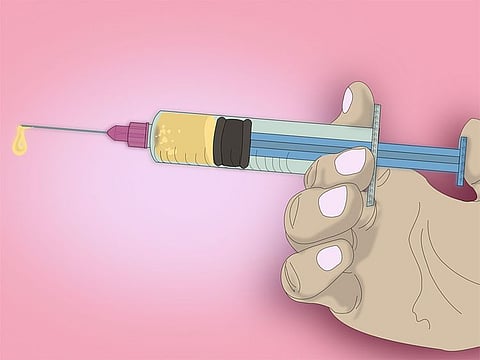
1. Therapeutic treatments (in addition to what we already have for the most sick patients) will arrive before vaccines. When someone contracts the novel coronavirus, his or her body’s immune system launches a defence, including producing antibodies that circulate in the blood to help identify infectious invaders.
These circulating antibodies offer some protection against future infection (for how long, we still don’t know). Scientists have now engineered clones of these antibodies — what we call monoclonal antibodies — and they are showing to be effective both therapeutically and to prevent infection.
They work by attacking the spike protein of the coronavirus, which is how this virus gets into our cells. Stop that from happening, and the virus can’t replicate inside the body.
Also a reminder that this is lightning-fast; if we get a vaccine within 12 months, that will be the quickest vaccine ever developed — by several years. There is an important caveat: My colleague Juliette Kayyem likes to point out that vaccines don’t save people, vaccinations doJoseph G. Allen
2. Rapid, low-cost saliva tests are also coming, and, as my colleague Michael Mina and Laurence Kotlikoff recently pointed out, they are a game-changer. Why? These are like home pregnancy tests but for covid-19, the disease caused by the novel coronavirus.
Imagine a test you could take at home every day, that gives you an answer in a few minutes after spitting into a vial. Such a test would change our ability to slow outbreaks where early detection is everything. It would also help consumer confidence and slow down this economic crisis.
Want to go to school or work or a Broadway production? Show that your rapid test was negative. These tests are not perfectly accurate, but the counterintuitive part is that they don’t have to be. More important than accuracy are speed and frequency of testing.
3. The debate is finally over: Masks work. It took three months, but widespread mask-wearing is catching on. What was once awkward and unusual (in the United States, anyway) has now become more accepted. More states and businesses are requiring them.
And, what was once political — thanks to the US president who said people were wearing masks only to make him look bad — is quickly becoming common sense. We now see leaders in red states urging mask-wearing. (Not all masks are created equal, so fortunately, there is now guidance on what constitutes a good mask.)
4. Consensus has finally emerged that airborne spread is happening. Scientists in my field have been warning about this for months (I have argued that airborne transmission is linked to super-spreader events), yet the Centers for Disease Control and Prevention and the World Health Organisation have consistently failed to recognise this.
This week, the tide turned when 239 scientists signed a letter to the WHO urging it to acknowledge airborne transmission. And that’s exactly what the WHO did.
This means that there will be more messaging coming out from the WHO and other organisations recommending that people add a new control to their toolkit for fighting this virus — healthy building strategies, such as higher ventilation, better filtration and the use of portable air-cleaning devices.
5. There is some science showing that past exposure to common-cold coronaviruses might be playing a protective role for some people.
This is a big claim — and I should caution that it is not fully resolved — but several studies are now showing that 20% to 50% of people who had never been exposed to the novel coronavirus have immune cells — known as memory T cells — in their body that react to this new virus. The speculation is that this is due to prior exposure to common-cold coronaviruses.
We still don’t know why some people fare better than others, or why a few spread the disease to many while others do not spread it at all, but these findings might hold some answers to those questions.
6. Vaccine trials seem to be working, and drug manufacturers have already said they might be able to deliver doses by October. Remember, it was not a given that vaccines would work, so the fact that the early-stage clinical trials are showing positive signs is encouraging.
Also a reminder that this is lightning-fast; if we get a vaccine within 12 months, that will be the quickest vaccine ever developed — by several years. There is an important caveat: My colleague Juliette Kayyem likes to point out that vaccines don’t save people, vaccinations do.
Once we have a vaccine, the hard task of manufacturing and distributing it comes into play. So, while the signs on vaccines are good, and we might have data in hand in a few months that they work, it will still be a few more months until people have the opportunity to actually receive the vaccine.
For the first time in history, nearly every scientist in the world is focused on the same problem. This is starting to pay real dividends.
Joseph G. Allen is an assistant professor of exposure assessment science, director of the Healthy Buildings program at Harvard University’s T.H. Chan School of Public Health and co-author of “Healthy Buildings: How Indoor Spaces Drive Performance and Productivity.”
Washington Post









