Risks of declaring the pandemic over too soon
We need to ensure that when we move on from Covid, we are prepared for future outbreaks
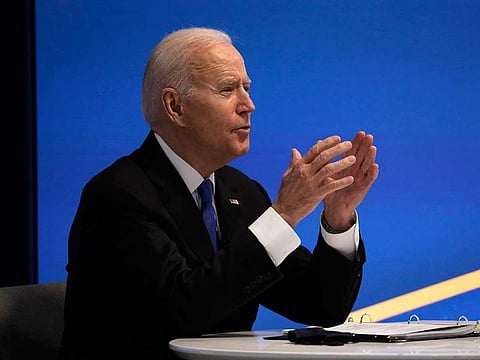
“The pandemic is over.” When “60 Minutes” aired recently, US President Biden shocked viewers by declaring an end to the Covid-19 pandemic.
How could a disease that has caused over 6.5 million deaths worldwide and continues to kill hundreds each day — even amid a recent push for more booster vaccines — be considered “over”? The backlash against Biden was expected.
The practice of a leader declaring an end to a pandemic — as if their words have the power to will contagion out of existence if they declare its conclusion — is not new. But sometimes such declarations prove to be premature, leading to relaxation of preventive measures and the unwillingness to take essential actions to prevent the next pandemic.
From the earliest pandemics in the American colonies, leaders have declared them over. For example, 300 years ago, a smallpox epidemic concluded in Boston.
Like most epidemics in the 18th century, it was sparked when a ship arrived with sick sailors, leading to a major outbreak in the spring of 1721. Smallpox spread, infecting approximately 6,000 inhabitants (out of a population of nearly 11,000) and leading to almost 850 deaths before its “end” in February 1722.
Hastening its end was a project of inoculation. Knowledge that inoculation could prevent the mortality of smallpox came from an enslaved servant of the Puritan clergyman Cotton Mather. Soon the local Dr. Zabdiel Boylston, a supporter of inoculation, and Dr. William Douglass, a denier of the process, were battling to be heard by the public.
As the epidemic infected at least one member of nearly every household in Boston, Boylston and Douglass fought over the best way to prevent more deaths. Soon Boylston had inoculated about 280 people.
In the 18th century, the end to an epidemic was one that was felt abruptly by city inhabitants. The disease had run swiftly through the local population, infecting — and in about 14 per cent of cases, actually killing — anyone who was susceptible.
With the speed of infections like smallpox, the disease would fizzle out when it had killed everyone it could and herd immunity had finally built up. In Boston, the decline of infections led to townspeople assuming the epidemic was over.
On Feb. 24, 1722, a town selectman shared with the city that no new cases of smallpox had been found that day, declaring it to be the official end of the epidemic. Many of Boston’s citizens still had smallpox; the numbers were just in decline.
Boylston published a piece on the process of inoculation and news of the process spread across the colonies. Yet, the push to inoculate children to prevent a future outbreak was halted as people assumed the threat was over and lost interest. As a result, three more major outbreaks happened in Boston, the next in 1752.
When it came to insect-borne diseases like yellow fever, the first frost often ended the spread of the disease as the mosquito vectors perished. Like a fire, contagion raced through city spaces, leaving as suddenly as it arrived, its consequences rippling for months to years afterward.
Yet city leaders still declared an official end to such outbreaks. In 1793, after an outbreak of yellow fever outbreak wreaked havoc on Philadelphia’s population for four months, the mayor declared the “end” of the scourge. Celebrations ensued — all while people were still rumoured to be sick.
Premature declarations of the end of outbreaks had consequences. After the yellow fever outbreak was considered over in Philadelphia, plans to open a second hospital, keep the streets clean and build a support system for orphaned children were cast aside.
Three more outbreaks, in 1795, 1797 and 1798, ravaged the Philadelphia community. It wasn’t until the early 1800s that funding and support were mobilised to bring public sanitation and citywide plumbing to the city.
Communities did not accept mass inoculation against smallpox until the 1770s, when George Washington, then the commander of the Continental Army, implemented a program to help the Revolutionary War effort. Doing so prevented future smallpox outbreaks.
Does Biden have a right to say that the epidemic is over? On Tuesday, Dr. Anthony S. Fauci explained that Biden’s declaration was really just an acknowledgement that the worst part of the pandemic was over. Still, Biden’s statement points to how leaders have thought about the end of epidemics for hundreds of years.
Communicating that the worst is over instills hope and optimism politically and socially, especially to a country that might be entering the fall and winter months with pessimism and disease fatigue. But the history of past epidemics reveals the messy ambiguity surrounding when a pandemic really ends — and who continues to experience the burden of the disease even after the emergency fades.
Considering the pandemic “over” might result in repercussions like the withdrawal of funding to support those whose lives were destroyed by long-term covid effects, medical bills, unemployment or lost loved ones.
This is a pivotal moment. We need to ensure that when we move on from this pandemic, we are prepared for future outbreaks and do not revert to protocols that were not successful at containing disease in the first place.
Declaring the end to an epidemic should be a moment to reflect on how we aid our communities, not an occasion to leave them behind as we move on.
Washington Post
Molly Nebiolo is a history scholar at the Northeastern University
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox



