Search for COVID-19 cure: Coronavirus’ possible weak spot found
Discovery of Achilles heel of the virus could help in developing therapies and vaccines
The discovery of a possible weak spot in the coronavirus has buoyed the search for therapies and vaccines. Scripps Research reported on Friday that a specific area of the virus could be vulnerable to drugs.
The spot “is a possible Achilles heel”, said Ian Wilson, the biologist who led the team that made the finding. This area is crucial in the spread of the pathogen, and its chemical composition indicated a vulnerability, giving rise to hopes that drugs could target the area. Scripps scientists also believe the discovery could also help develop a vaccine, the San Diego Union-Tribune reported.
While examining an antibody from a SARS patient, Wilson found that it latched onto a particular place in the virus. Scripps’ scientists found that the SARS antibody clung onto to the exact spot on the coronavirus too.
“That high degree of similarity implies that the site has an important function,” Scripps Research said in a statement, adding that more research is needed.
The finding was published in the journal Science.
The search for a cure continues
With the new coronavirus spreading like wildfire, scientists are racing to find therapies. Time is of the essence. So the search for drugs to treat COVID-19 is focusing on antivirals in the market.
Researchers are also looking at repurposing medications used to treat other diseases. This is a faster way to find therapies than creating a new drug to fight COVID-19, says Nevan Krogan, a biologist at the University of California, San Francisco.
“I think it takes an average of at least six years in order to come up with a drug, but if we can use drugs that exist for other diseases and repurpose them, we may have drugs that we could be using right now,” Krogan told ABC News.
In the absence of a cure, a cocktail of antiviral drugs is used to treat critically-ill patients. Doctors in China, Australia and India are reported to have cured patients with medicines to treat HIV and malaria. In China, they have incorporated traditional herbal medicines into their therapies.
In a bid to tweak available medications, a team of scientists have drawn up a list of 69 medicines and experimental compounds which may work against the virus, reports said.
The list published on the website bioRxiv includes medicines used to treat unrelated diseases as cancer, Parkinson’s, hypertension, schizophrenia and Type 2 diabetes.
How the virus targets human cells
Hundreds of scientists, led by Krogan, studied 26 of the coronavirus’ 29 genes responsible for producing viral proteins. So researchers looked at drugs that latch onto the human proteins targeted by the coronavirus to replicate in human cells. And they identified 69 drugs and compounds that could be useful to combat the coronavirus.
Haloperidol (used for schizophrenia), metformin (used against Type 2 diabetes) and anti-malarial drug chloroquine (used by Indian doctors in Rajasthan) are among the drugs that figure in the list.
Favilavir, the only approved coronavirus drug
Favilavir is the only approved drug for the treatment of coronavirus. But only in China. The antiviral drug, originally designed to treat inflammation of the nose and throat, received approval from Chinese authorities for COVID-19 treatment after it reportedly helped cure the disease in a clinical trial involving 70 patients in Shenzhen, Guangdong province.
Last month, Taizhou's city government declared that Favilavir, formulated by Hisun Pharmaceutical in China, as the first medicine authorised to stop the global pandemic. The drug – also known as Avigan – was developed by Fujifilm Toyama Chemical in 2014. A Japanese health ministry source suggested the drug was not as effective in people with more severe symptoms, indicating the need for more data.
The drug is yet to be approved by the US Food and Drug Administration (FDA).
Ivermectin, the new drug on the block
The antiparasitic drug is the latest to show promise as a coronavirus treatment. Ivermectin, used for years to treat a range of conditions including head lice and scabies, has been found to kill SARS-COV2 in a controlled lab within 48 hours, reports from Australia say, following a study by the Monash Biomedicine Discovery Institute and the Peter Doherty Institute for Infection and Immunity in Melbourne.
Ivermectin, approved by the US Food and Drug Administration, has been effective against a broad range of viruses including HIV, dengue, influenza and Zika.
Clinical trials could be at least a month away, according to Kylie Wagstaff, who led the study. But before that, it has to be determined whether Ivermectin can treat coronavirus in humans, and what would be a safe dosage.
The lure of chloroquine
Chloroquine, a synthetic version of quinine, has been used to treat malaria for nearly a century. The drug was in the news in the United States after President Donald Trump seemed to back its use at a news briefing at the White House last month. He also tweeted that the combination of chloroquine and antibiotic azithromycin together can be “a game-changer in the history of medicine”.
Dr Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in the US, was quick to warn that there was only “anecdotal evidence” of chloroquine’s effectiveness.
At least two dozen trials are underway in China. New York is also trialling chloroquine in combination with antibiotic azithromycin. The early results are encouraging, but positive cell study results with chloroquine against viral diseases, dengue and chikungunya, didn’t lead to a cure.
Chloroquine is cheap and is safe for humans, though at higher doses it can result in poisoning. It’s also been effective against severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and human immunodeficiency virus (HIV), which is the reason for its appeal.
Azithromycin is on the ascendancy
Azithromycin seems to find favour among the French researchers. They used the antibiotic in combination with the anti-malarial medication hydroxychloroquine, according to research published in the International Journal of Antimicrobial Agents.
The case for hydroxychloroquine
Closely related to chloroquine but less toxic, hydroxychloroquine has been used to treat autoimmune diseases like lupus and rheumatoid arthritis. Recent lab results seem to attest to its efficacy against the coronavirus.
Hydroxychloroquine has been on the market since the 1950s. At least seven clinical trials in China are verifying its usefulness against the coronavirus, besides another trial in the University of Minnesota. The early results are promising.
Kaletra, the combo drug
Kaletra is a combination of two antiviral drugs, lopinavir and ritonavir, which have different but complementary roles when used against HIV. Researchers hope to disrupt SARS-COV-2 similarly, but a study published the New England Journal of Medicine reported no benefit.
Several clinical trials are underway, and they could provide more insight.
Remdesivir: Is it a mirage?
Originally developed to fight Ebola, remdesivir had shown encouraging results in tests against coronaviruses that cause MERS and SARS. Scientists aim to replicate that success against SARS-COV2, although there has been no proof yet.
A case study published in the New England Journal of Medicine gives us a glimmer of hope. Remdesivir was administered to a COVID-19 patient in the United States after his condition started deteriorating. The patient’s health began to improve the next day, but it’s not known whether Remdesivir helped in the recovery.
A Californian patient, who doctors thought might not survive, recovered after being treated with remdesivir. Such individual cases don’t prove a drug is safe and effective, but the clinical trials at several locations in the US should provide a definite answer.
Losartan on trial
Scientists believe this hypertension drug can help COVID-19 patients because of the way it reduces blood pressure. Losartan is trialled at the University of Minnesota.
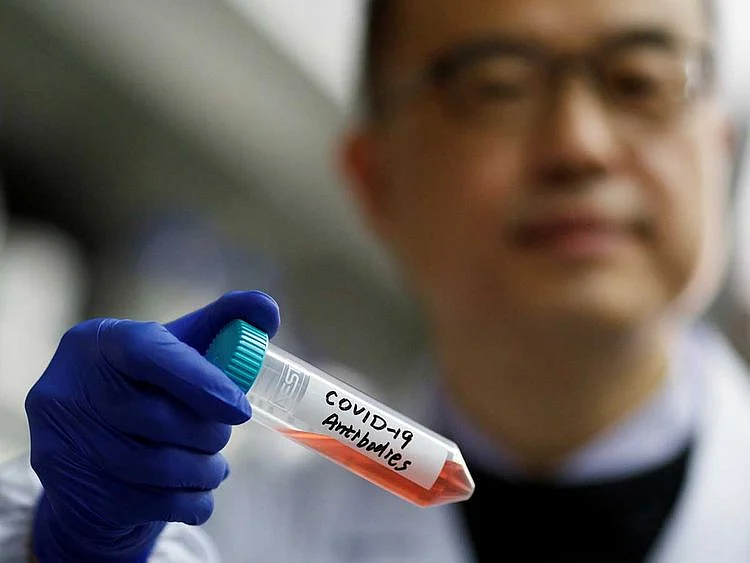
Plasma therapy in focus
More studies have shown that infusions of antibody-rich plasma from recovered patients (also called convalescent plasma) help in treating people infected with the coronavirus. The technique of convalescent plasma, first used in the 1890s against diphtheria, seems to work against COVID-19 too.
A pilot study conducted at three hospitals in China suggested the benefits of harvesting antibodies from recovered people and administering it to people battling COVID-19. The preliminary findings were published in the journal PNAS, the Proceedings of the National Academies of Sciences.
A report in the Journal of the American Medical Association last month also showed that five critically ill patients in Shenzen, China, recovered after treatment with plasma.
Japanese drugmaker Takeda Pharmaceutical Co. said it was developing a new drug from the blood plasma of people who have recovered.
The therapy has potential, but researchers say that only more extensive and detailed studies will help shed more light on the healing effects of convalescent plasma.
The other approach
Repurposing approved antiviral drugs may be a good start considering the urgency, but it’s not a preferred route, scientists say. So researchers are also studying the virus minutely to develop precise treatments from scratch. The downside to it is that it may take longer, much longer, to bring a drug to the market.
Scientists are looking to resume the studies in SARS and MERS that were discontinued after their threats faded. Since all three coronaviruses (which cause SARS, MERS and COVID-19) are genetically similar, that preliminary work could shorten the process of developing a drug to around 12 to 18 months, says Karla Satchell, professor of microbiology-immunology at Northwestern University’s Feinberg School of Medicine in Chicago, Illinois.
It’s imperative to continue the research even after the current pandemic ends, Satchell says, adding that if the work into SARS and MERS had resulted in effective drugs, we might have a treatment for COVID-19 today.
The future
All these medicines are in various stages of experiments and trials. People should not use these drugs without medical advice. Many of them have serious side effects, and some could even be fatal.
A cure is still a long way off. The speculation is that by the time a treatment is found, COVID-19 would have ceased to be an epidemic. But scientists should heed Satchell’s words and continue their good work.
It will help fight future outbreaks.
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox
Network Links
GN StoreDownload our app
© Al Nisr Publishing LLC 2026. All rights reserved.