COVID-19 causes blood clots harming organs from brain to toes
If clots go untreated, they may manifest days to months after respiratory symptoms
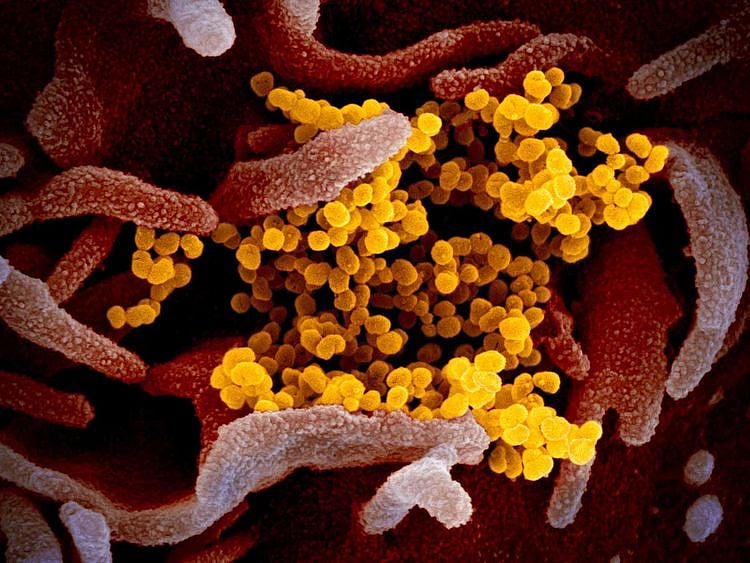
Another threat from the lung virus that causes COVID-19 has emerged that may cause swift, sometimes fatal damage: blood clots.
Doctors around the world are noting a raft of clotting-related disorders - from benign skin lesions on the feet sometimes called "Covid toe" to life-threatening strokes and blood-vessel blockages. Ominously, if dangerous clots go untreated, they may manifest days to months after respiratory symptoms have resolved.
The clotting phenomenon is "probably the most important thing that's emerged over the last perhaps month or two," said Mitchell Levy, chief of pulmonary critical care and sleep medicine at the Warren Albert School of Medicine at Brown University in Providence, Rhode Island.
It's not unusual for infections to raise the risk of clotting. The 1918 Spanish flu pandemic, caused by a novel strain of influenza that killed some 50 million people worldwide, was also linked to downstream damage from clots that could end lives dramatically.
Viruses including HIV, dengue and Ebola are all known to make blood cells prone to clumping. The pro-clotting effect may be even more pronounced in patients with the coronavirus.
"There's something about this virus that's exaggerated that to the nth degree," said Levy, who is also medical director of the medical intensive care unit at Rhode Island Hospital. "We're seeing clotting in a way in this illness that we have not seen in the past."
The problem is visible in clots - doctors call them thrombi - that form in patients' arterial catheters and filters used to support failing kidneys. More pernicious are the clots that impede blood flow in the lungs, causing difficulty breathing.
Rapid deterioration
These are probably what's causing patients who otherwise appear well to suddenly "fall off the ledge" and develop severe blood-oxygen deficiency, said Margaret Pisani, an associate professor of medicine at the Yale University School of Medicine in New Haven, Connecticut.
Clotting disorders in COVID-19 patients were noted by researchers in China in February, but their gravity has since become clearer. While doctors had thought the vast majority of lung damage was due to viral pneumonia, they're now looking more closely at clotting.
"When you look at autopsies now, we are seeing things that we didn't expect," said Anthony Fauci, the director of the National Institutes of Allergy and Infectious Diseases who's at the forefront of the US pandemic response. Clumps of platelets inside blood vessels, or microthrombi, are probably why Covid patients can "rapidly and dramatically deteriorate," he said in an interview with CNN last week.
Separate studies from France and the Netherlands found that as many as 30 per cent of severely ill COVID-19 patients suffered a so-called pulmonary embolism - a potentially deadly blockage in one of the arteries of the lungs. These often occur when bits of blood clots from veins deep in the legs travel to the lungs. By comparison, the prevalence of pulmonary embolism was 1.3 per cent in critically ill patients without COVID-19, one study found.
Cardiac arrest
If untreated, large arterial lung clots can put overwhelming strain on the heart, causing cardiac arrest. Even tiny clots in the capillaries of lung tissue may interrupt blood flow, undermining attempts to help oxygenate patients with ventilators, said Edwin van Beek, chair of clinical radiology at the University of Edinburgh's Queen's Medical Research Institute.
In the early 1990s, Van Beek helped develop the D-dimer blood test that's used around the world to monitor clot formation in patients, including those with COVID-19, and to dose them with heparin and other anticoagulant medications.
Untreated pulmonary embolism is lethal in one in three cases, and will recur in another third, he said. In 3 per cent to 7 per cent of patients, it will cause pulmonary hypertension, another dangerous complication that can cause fatigue and shortness of breath.
Scarred lungs and clotting-related problems may be a lingering legacy of the pandemic, Van Beek said. COVID-19 survivors who have subsequent difficulty breathing, especially on exertion, might mistakenly believe it's a recurrence of coronavirus infection, when it may actually be a "reactivation of the whole clotting problem."
"I expect to see more of this as we come out of the pandemic," he said. Patients and doctors alike may not be aware of the risks or the potential need for treatment.
Coagulation may occur because of damage to cells lining blood vessels that results from both the viral infection and the immune system's inflammation-causing response, said Jean Connors, a Harvard Medical School hematologist.
"The outcome isn't affected if you're treated appropriately," she said. But "it's possible that people are dying from undiagnosed pulmonary emboli."
Organ damage
Clots may form in other parts of the body, potentially damaging vital organs including the heart, kidneys, liver, bowel, and other tissues.
Five cases of stroke were treated in Manhattan's Mount Sinai Health System over a two-week period through early April, doctors reported in the New England Journal of Medicine last week. The patients, who all had the coronavirus and were younger than 50, were treated for large-vessel blockages.
It's a rare complication amplified by the "sheer numbers of infected patients," Connors said. New York City has reported about 170,000 COVID-19 cases, including roughly 43,000 hospitalisations.
Puzzling, enlightening
Such findings are "puzzling" on one hand, "but on the other hand are enlightening" because they can inform better ways to treat patients, said Fauci, the NIAID leader.
In Italy, the first European country gripped by the pandemic, it was after COVID-19 patients died from acute pulmonary emboli and other clotting-related events that doctors moved to inflammation-blocking treatments, such as tocilizumab, sold by Roche Holding AG as Actemra, said Frank Rasulo, a head of neuro critical care at Spedali Civili University Hospital in Brescia.
Some doctors are starting to see COVID as less of a typical respiratory disease, and more of one that involves dangerous clotting, said Rasulo, who is also an associate professor of anesthesia and intensive care. "That's quite frightening when you think of it, because we didn't know what we're up against until we were in a later stage."
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox
Network Links
GN StoreDownload our app
© Al Nisr Publishing LLC 2026. All rights reserved.