R0: What to know about viral infection rate
As more people take precautions, the rate goes down; otherwise, the reverse kicks in
Also In This Package
Mosaic of Hope: Portraits of people wearing face masks
From the editors: COVID-19 tests at cheaper rates
9 months on: All we know about COVID-19 and pregnancy
In Pictures: Madrid fashion week kicks off
Trouble setting financial goals during COVID-19?
From the editors: Quick takes from the day's events
Meet the Vietnamese billionaire helping COVID-hit world
Landed in Dubai, do I need to quarantine in Abu Dhabi?
DUBAI: Health experts, policymakers and citizens are all watching the coronavirus reproductive number (called R0, or R zero, aka R=nought) closely. But what is it?
What does it mean, really?
There’s so much going for the ‘R’ ("reproductive number"). In the case of the novel coronavirus (SARS-CoV-2), the pathogen that causes COVID-19, the number goes up and down.
What's more, those numbers are carefully considered when restrictions — and easing of those restrictions — are announced and imposed on the community.
As it turns out, R0 is the key. Policy makers use it when figuring out how soon can people go back to their normal routine: work, school and holidays.
What is an R0?
The basic infection reproduction number is meant to be an indicator of the contagiousness or transmissibility of infectious and parasitic agents.
In epidemiology, it’s a common metric used to describe the contagiousness — or "transmissibility" — of pathogens (disease-causing agents like bacteria, viruses).
During an epidemic, R0 refers to the basic reproduction number. It is also called the “basic reproduction ratio” or rate or the “basic reproductive rate”.
R0 IN MOVIES
The 2011 movie “Contagion,” about a worldwide pandemic of a new virus, the term “R0” has been used a lot. Also in the movie "Outbreak" (1995), about a deadly virus carried by a monkey host from the African rain forest, which started infecting the entire population, a handful of scientists struggle to find a cure.
Where did the concept come from?
Demographers first used and introduced the concept of R0, when the metric was used to count offspring.
When R0 was adopted for use by epidemiologists, the objects being counted were infective cases.
What is the formula for computing the R0?
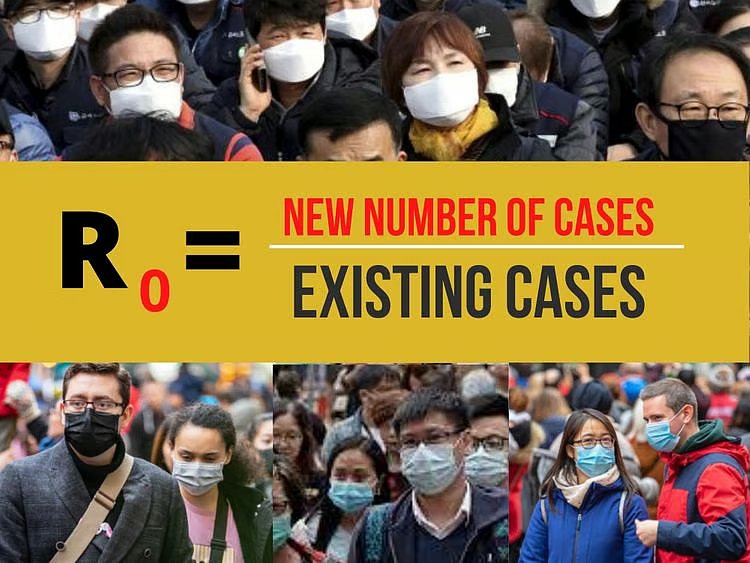
The value for R0 is equivalent to the nuber of new cases over existing cases, according to the Emerging Infectios Diseases journal.
Can you give me a number of scenarios on how I can compute R0?
Below is a rather simple example, with four scenarios, provided by a CDC expert.
(1) Let's say you're analysing 4 types of infections (A, B, C, D).
What are the various factors involved in calculating R0?
The computation of R0 is affected by numerous factors, including:
These factors govern pathogen transmission. Demographers and bio-statisticians usually estimate R0 with various types of complex mathematical models.
A study published in January 2019 cautioned that due to its complexity — and considering the socio-behavioral, biological and environmental factors involved — R0 is easily "misrepresented, misinterpreted, and misapplied".
WHAT R0 IS NOT
R0 is not a biological constant for a pathogen, a rate over time, or a measure of disease severity, and R0 cannot be modified through vaccination campaigns. [Source: Emerging Infectious Diseases, https://bit.ly/2RiIjNk]
When is it best to use R0 – what pitfalls need to be considered?
This basic metric is quite useful, but it's far from simple: R0 must be estimated, reported, and applied with great caution, warn experts.
A team led by medical geography specialist Dr. Paul Delamater of the University of North Carolina at Chapel Hill wrote “Complexity of Basic Reproduction Number (R0)” in the Emerging Infectious Diseases journal explaining the pitfalls of R0 calculations. The team explained that "R0 is rarely measured directly".
Moreover, the team stressed that modeling R0 values are dependent on model structures and assumptions which may no longer be valid, especially when considering the relevance or applicabaility of historical data to the present period.
At what point does an outbreak continue, or stop?
Because the R0 for an infectious disease event is generally reported as a single numeric value (or low–high range), an interpretation of R0 is typically presented as straightforward.
So for example, an outbreak is expected to continue if R0 has a value >1 (greater than 1) — and to end if R0 is <1 (less than 1).
The potential size of an outbreak — epidemic/pandemic — often is based on the magnitude of the R0 value for that event. The graph below shows the R0 for different infectious diseases. The farther to the right you go, the higher the infectiousness/contagiousness. The higher you go, the high the mortality rate.
R0 values have been published for measles, polio, influenza, Ebola virus disease, HIV disease, a diversity of vector-borne infectious diseases, and many other communicable diseases.
R0 can also be used to estimate the proportion of the population that must be vaccinated to eliminate an infection from that population.
R0 values have been published for measles, polio, influenza, Ebola virus disease, HIV disease, a diversity of vector-borne infectious diseases, and many other communicable diseases.
Why is it difficult to determine R0?
On the surface, R0 looks quite simple to calculate. But the models used in guiding the estimates must use exhaustive scientific measures. And this is the difficuylt part. Most of the R0 estimates almost always are based retrospectively from seroepidemiologic data or by using theoretical mathematical models.
Data-driven approaches include the use of the number of susceptible persons, average age at infection, final size equation, and intrinsic growth rate.
When mathematical models are used, R0 values are often estimated by using ordinary differential equations. This makes high-quality data rarely available for all components of the model.
Often estimated values of R0 generated by mathematical models are dependent on numerous decisions made by the modeler. This is further complicated by
The following critical model parameters and sub-parameters must also be considered, such as:
Other decisions include whether to use a deterministic (yielding the same outcomes each time the model is run) or stochastic (generating a distribution of likely outcomes on the basis of variations in the inputs) approach.
An important point cited by Delameter's team: Some of the R0 values commonly reported in the literature for past epidemics (might not be valid for outbreaks of the same infectious disease today.
Is it possible to get the true values for R0?
Delamater's team pointed out that many of the parameters included in the models used to estimate R0 are merely "educated guesses".
"The true values are often unknown or difficult or impossible to measure directly," they stated.
Experts say that in order to match the present-day epidemiologic reality, the calculation of the R0 must take into account the following:
Takeaways:
R0 data acquired during 1912–1928 need
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox
Network Links
GN StoreDownload our app
© Al Nisr Publishing LLC 2026. All rights reserved.