COVID-19: How long will the immunity against coronavirus last?
Severe infection produces antibodies, asymptomatic cases need not provoke immune response
An infection usually leads to immunity. So if you have been infected with the new coronavirus, SARS-Cov-2, you certainly would have developed immunity against COVID-19. How long will that immunity last? At least four months. More time and more studies are required to determine a more precise duration for the protection.
Several studies confirm that people who survive a COVID-19 infection will develop immunity, but the duration of the protection couldn’t be ascertained since it’s a new virus. A severe infection leads to a higher level of antibodies, while asymptomatic cases lose the antibodies faster, according to the findings by Imperial College London.
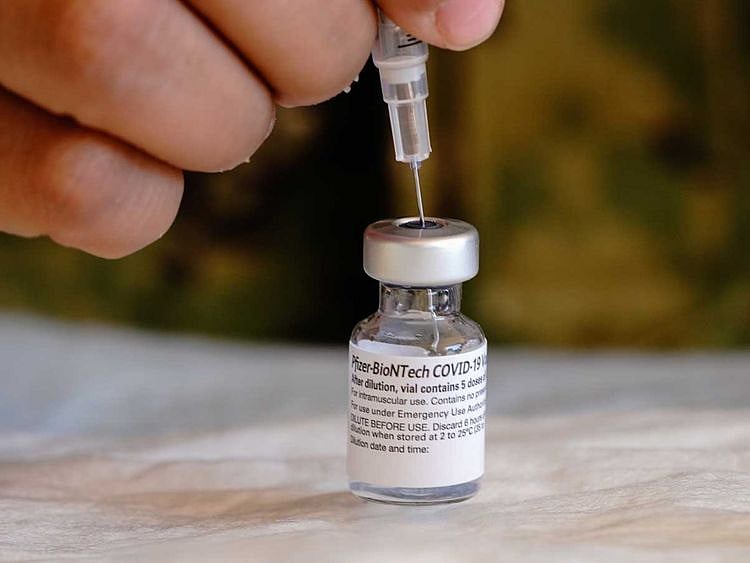
Since some people don’t develop adequate immunity, they have to be vaccinated against reinfection. That’s what the UAE government has decided.
“If the immunity tests are positive, they would not require vaccination. However, if antibodies are not formed, they would be given the vaccine,” Dr Omar Al Hammadi, an official spokesman said, adding that “the vaccination of infected people depends mainly on the recommendation and evaluation of specialists.”
Let’s take a look at immunity and immunity tests.
What’s immunity? How does it work?
Immunity is the body’s defensive mechanism to fight off invading pathogens and their harmful effects. It’s essential for our survival.
Innate immunity is the first line of defence against infections. It is a generic rapid response, but it does not last long.
Adaptive immunity is a specific response. It is acquired after exposure to a pathogen, and re-exposure to the same germs produces a more rapid immune response.
What are the factors that affect immunity?
A healthy lifestyle can enhance a person’s immune system, Dr Zeinb Sabri, internal medicine specialist at Medcare Hospital – Sharjah, said. Some disorders or conditions could impact immunity. “Chronic conditions like diabetes that is uncontrolled, or autoimmune diseases like rheumatoid arthritis, cancers, and diseases leading to immune deficiency disorders, like HIV, affect the immune response,” Dr Sabri added.
The ability of a person to produce antibodies is affected by their age, nutritional status and associated comorbidities, Dr Mirhan Alkady, specialist pathologist, and assistant medical director at Burjeel Specialty Hospital, said.
“Elderly people, or those suffering from a mineral or vitamin deficiency, are more likely to have impaired immune system response. People with chronic diseases – like chronic renal failure, liver cell failure and cancer – may also show delayed antibody response because of an inhibitory effect on the bone marrow,” Dr Mirhan added.
What are immunity tests?
Immunity tests or serology tests look for antibodies and immunoglobulins in the blood. They are also referred to as antibody tests. Actually, antibodies and immunoglobulins are similar, but not the same. For the sake of simplicity, we will use them interchangeably.
Note that that the immunity tests don’t look for the virus. It’s used to find out whether your immune system has responded to the infection (against the SARS-CoV-2).
What’s a COVID-19 immunity test?
The COVID immunity test hunts for immunoglobulins known as IgG, which would indicate lasting protection against the disease. IgG is a secondary response, and these antibodies are more specific to the virus or disease.
IgG antibodies are generated around 12 days after symptoms start. They can remain in the blood long after the infection goes away, but we don’t know how long that is for the new coronavirus.
IgM is usually the first antibody produced by the immune system when a virus attacks. It signifies an acute infection phase. When IgM is detected, it means the person is still infected, or have recently recovered from an infection.
How is a COVID-19 immunity test different from the PCR test?
The PCR (polymerase chain reaction) test, also called a molecular test, detects the genetic material of the coronavirus, while the antibody test detects the specific COVID-19 antibodies generated in response to the virus.
What’s an antigen test?
An antigen test identifies specific proteins in the coronavirus. The tests use the sample from a nasal swab and produce results in minutes. Antigens are substances or germs that provoke the immune system to generate antibodies.
The majority of rapid diagnostic tests have been antigen tests. They are useful for identifying a person with peak infection. Antigen tests are less expensive and generally faster.
How long will antibodies last?
All antibodies don’t have the same lifespan, Dr Sabri said. “For example, we need to take a new flu shot every year because the flu virus itself changes, whereas Hepatitis B immunisation lasts a lifetime. Others last for a shorter period: antibodies that cause meningitis (Neisseria meningitis) last for three years,” she added.
Why is COVID immunity period difficult to determine?
The SARS-CoV-2 is a new virus, so little is known about the immunity provided by the antibodies generated to battle a COVID infection. The virus has been around only for a year, so there hasn’t been enough time to ascertain the duration of the protection.
What do the studies say?
A study, which tracked antibody levels in Britain following the first wave of infections in March and April, suggested that the immunity may not last long. Researchers at Imperial College London found that the presence of antibodies decreased from 6 per cent of the population at the end of June to 4.4 per cent in September.
Two studies, published in the journal Science Immunology, showed that COVID survivors continue to have antibodies against the virus for at least three to four months after the infection.
The researchers found three types of antibodies 12 days after the infections. IgG offers potential to give sustained immunity. Two other antibodies, IgA and IgM, disappeared within two months. IgA protects against infection on respiratory and gastrointestinal tracts, and IgM is the first antibody generated to fight infection.
What are the chances of COVID reinfection?
The reports of reinfections are rare. That’s not to say it’s not possible. Most reports say that the second infection is from a different strain of the virus.
Since such reports are far and few, scientists believe acquired immunity after a SARS-CoV-2 infection offers adequate protection.
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox
Network Links
GN StoreDownload our app
© Al Nisr Publishing LLC 2026. All rights reserved.