First person: Why a possible HIV cure is not cause for celebration
News about a second person who may be free of virus is a distraction from work at hand
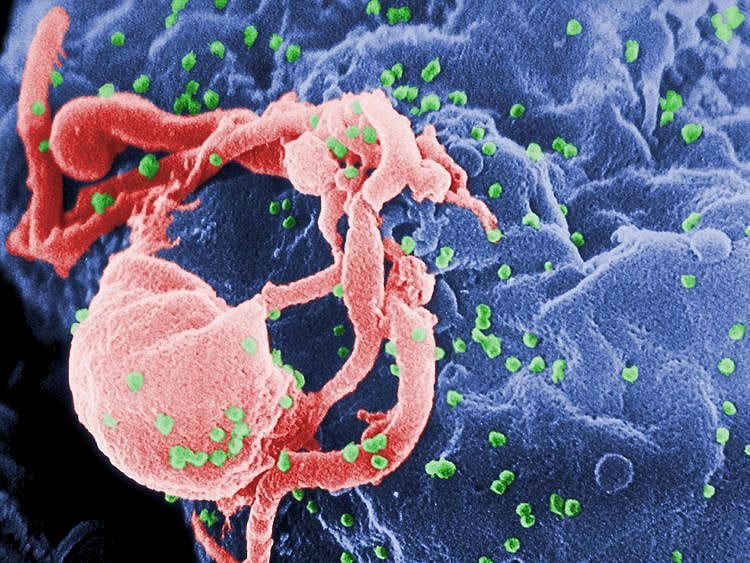
HIV is not going away anytime soon. I’ve been living with the virus for more than 20 years and have seen the overhyped stories promising a cure around the corner pop up regularly, particularly around the time of big Aids conferences.
The news recently that a second person seems to have gone into long-term remission from HIV after a stem-cell transplant is a real scientific advance.
But I fear the sensationalism with which this report was received could do more harm than good obscuring the actual struggles we face in combating this epidemic.
In the case reported recently, cancer was an opportunity that offered the chance to cure two diseases at once. The individual, known as the “London patient,” received the transplant from a donor with a genetic mutation that conferred resistance to the HIV infection.
He was the second person ever to sustain long-term viral suppression in the absence of anti-retroviral treatment.
Timothy Ray Brown, also known as the “Berlin patient,” underwent a similar procedure 12 years ago, with the same remarkable results.
But stem-cell transplants from these rare donors are unlikely to be used for the average HIV-positive patient without cancer, because of the risks involved and the impracticality and costs of these procedures.
In reality, a cure for HIV remains a distant dream and the focus on the two “cured” patients is a distraction from the hard, far less headline-grabbing work that we still have to do.
In 1995, I was at the bedside of my cousin Carl, who was dying of Aids. His siblings, my aunt and I tended to him during his illness. It was the most terrible period in my life.
HIV positive
That year was also the year I also found out I was HIV-positive. I was 32. My first laboratory results were not encouraging. My T-cell levels were quite low, which meant my disease was already progressing towards the danger zone where I would be at risk of infections like those that killed my cousin.
Since 1981, this disease had been a death sentence for most people who were HIV-positive, and I had few hopes for my own survival.
But then a miracle happened. There was a great leap forward in Aids treatment soon after Carl’s death. People desperately ill came back from the brink, and the new treatment began to offer a normal lifespan for others of us living with HIV.
Within a few years, the death rate from HIV plummeted in the United States and in the global north. By the end of the decade, a sweeping campaign began to reduce the prices of these new drugs and to get them to patients across the globe.
This all came too late for Carl, but just in time for me and a generation of people living with the virus.
It is one of the great honours of my life that I got to work with the tireless activists who battled governments and drug companies to make this all happen.
From the late ‘80s, along with my colleagues in ACT UP (Aids Coalition to Unleash Power, an international direct action advocacy group) and the Treatment Action Group, I fought for investments in Aids research and drug development and changes in the way both were done.
Delivery of HIV care
By 2000, I had moved on to pushing for access to medicines in the global south. However, I made the decision in 2008, in my mid-40s, to go back to college.
Since then, I have been working on solving the fundamental operational problems facing the delivery of HIV care and dealing with the opioid epidemic and infectious diseases like hepatitis C that, along with HIV, can travel in its wake.
While we should continue to dream big and hope for a cure, my own history has shown that a few months in the here and now can make the difference between life and death.
As researchers and activists, we have to urgently focus on what works, on overcoming barriers to scale up HIV treatment and prevention, which will need both scientific and political solutions.
The recent study may be an important step in getting us a cure for all.
But, there is so much more to do to ensure that the promise of discoveries now more than 20 years old — these powerful Aids drugs — become a reality for millions today who will perish, like my cousin Carl, without them.
— New York Times News Service
Gregg Gonsalves is an assistant professor at the Yale School of Public Health
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox
Network Links
GN StoreDownload our app
© Al Nisr Publishing LLC 2026. All rights reserved.