How black fungus infections are maiming COVID-19 patients in India
Health minister urges early diagnosis amid rise in cases of deadly mold across India
Dubai: Doctors in India are reporting a rush of cases involving a rare and deadly fungus that erodes facial structures of COVID-19 patients and fatally damages the brain, prompting an advisory from the Indian health minister and a scramble for an anti-fungal injection that is the only known cure for it.
Although a rare infection, mucormycosis or black fungus is increasingly being detected among post-COVID-19 patients even as India battles to contain a massive outbreak of virus cases.
Medical experts said the fungus seems to be infecting recovered COVID patients with weakened immune systems due to high intake of steroids, and underlying health conditions such as uncontrolled diabetes.
High mortality rate
“We are getting at least five patients every day with loss of vision, nasal blockage and pain in the cheeks,” Dr Rakesh Srivastava, president of the Association of Otaryntologists of India (Lucknow chapter) and senior consultant at SIPS Specialty Hospital in Lucknow, told Gulf News in a phone interview. “These symptoms typically manifest 10-15 days after the COVID-19 infection has receded. This is a fungus that blocks capillaries and melts tissues… Since it can attack through the respiratory tract, potentially eroding facial structures and damaging the brain, mucormycosis has a very high mortality rate,” he said.
According to Dr Srivastava, a large majority of the cases require aggressive medical surgeries such as removal of an infected eye, the entire orbital wall, or the jaw bone. “We have to remove every infected area just to save the patient’s life. But even then, the chances of recovery are low for almost every diabetic patient who contracts the fungus and develops complications,” he said.
Spreading through states
In the western state of Maharashtra, local media reported that more than 200 recovered COVID-19 patients were being treated for mucormycosis and that eight had died. Haryana’s Health Minister Anil Vij on Saturday said black fungus has been declared a notified disease in the state after 27 cases surfaced – mandating any diagnosis to be reported to the district chief medical officer. Cases and deaths from the fungal infection have also been reported in New Delhi, Gujarat, Karnataka, Telangana and other places which have recently seen a surge in Covid-19 infections.
“The cases of mucormycosis in COVID-19 patients post-recovery is nearly four to five times than those reported before the pandemic,” Dr Atul Patel, an infectious diseases specialist and a member of Gujarat’s COVID-19 taskforce, told AFP.
Diabetics at high risk
While some experts have attributed the spike in fungal infections to an increased use of steroids to treat hospitalised COVID-19 patients, others have pointed to families applying oxygen therapy at home without proper hygiene.
But Dr Srivastava said that several of his black fungus patients in Uttar Pradesh – of which Lucknow is the state capital – have been in home isolation and have never been to any hospital and never taken oxygen supplies. “This is mainly prevalent in pre-diabetics as well as uncontrolled diabetics. But it doesn’t spread from one person to another,” he said. More than 10% of India’s adult population – or 77 million people – are estimated to be diabetic.
Warning from Indian health minister
The sharp rise in cases prompted Indian health minister Dr Harsh Vardhan to urge people on the early detection and management of mucormycosis. “Awareness and early diagnosis can help curb the spread of the fungal infection,” he tweeted on Friday.
The situation is also rapidly straining the inventory of Amphotericin B – the expensive anti-fungal drug used to treat black fungus. “Every day we are getting new cases, but we don’t have enough supplies of Amphotericin. This is the case in other states too,” said Dr Srivastava.
All you need to know about Black Fungus
What is Mucormycosis?
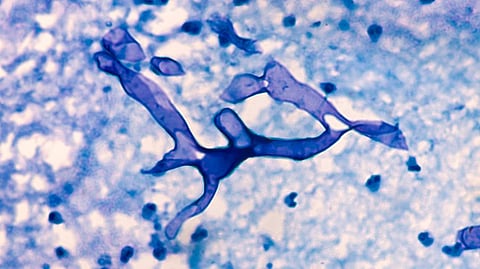
Mucormycosis is caused by a family of molds called mucormycete (black fungus), which grow in soil and decaying organic matter, such as rotting leaves and wood, according to the US Centres for Disease Control and Prevention (CDC). The fungal spores are ubiquitous and found in soil, air and even in the nose and mucus of healthy people. The fungal infections are also common in places where there’s a lot of earth-moving construction work going on.
How does the fungus infect the human body?
The fungus is typically inhaled – getting into the sinuses or lungs and deposited there after people breathe in the fungal spores. The mold can also enter the body through cuts and other abrasions in the skin. Once inside the body, the fungus can sometimes spread through the bloodstream and affect organs such as the eyes, spleen and heart. They also get into the air spaces in the head and invade the base of human brain – where it becomes an extremely critical infection.
Why is it happening in COVID-19 patients?
While healthy people’s immune systems can usually fend off the fungus, COVID-19 is creating conditions for the fungal infection to take hold by compromising the human immune system. The rise in cases could also be connected to the high use of steroids in hospitalised COVID-19 patients, since the drugs suppress the immune system to treat inflammation caused by the virus. People with conditions such as uncontrolled diabetes or leukaemia – that severely weaken the immune system – are highly prone to the spores developing into an infection.
What are the symptoms?
• Pain and redness around the eyes and nose
• Stuffy or bleeding nose
• Swollen eyes
• Droopy eyelids or blurred vision
• Black patches on the skin around the nose
• Pain on one side of the face, in the sinuses and teeth
• Fever, headache and cough
What is the damage caused by the fungus?
Mucormycosis is expensive and difficult to treat, with a mortality rate upwards of 50 per cent. Many patients have their eyes or jaw bones surgically removed due to the infection. If the infection has spread, surgery is invariably needed to cut and clear out the source of the fungus – which is usually the sinus, the back of throat and even very delicate places like the base of brain. The fungus can be life-threatening in diabetic or severely immunocompromised individuals.
What is the cure?
Liposomal Amphotericin B, an anti-fungal intravenous injection which costs Rs3,500 (around Dh175) per dose and has to be administered every day for up to eight weeks is the only drug effective against the disease. Fluid and tissue samples may be taken to confirm a diagnosis.
Are there any precautions to prevent the infection?
According to the Indian Council of Medical Research and the Indian Health Ministry, people should:
• Immediately report any symptoms
• Not neglect any pains of the sinus
• Wear shoes, long trousers, long sleeve shirts and gloves while handling soil, moss or manure
• Maintain personal hygiene
• Ensure if they have diabetes that it is well controlled
• Should discontinue immune-suppressing drugs such as steroids as soon as doctors are able to
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox








