Rapid COVID-19 tests: What negative or positive results mean
Experts point to benefits of antibody tests, and their role in vaccine trials
Also In This Package
DUBAI: Authorities around the world are easing quarantine measures, though sometimes local lockdowns are re-imposed due to localised outbreaks.
With social distancing still in place, and daily news of infections and deaths, testing has become part of public discourse. Yet, there’s some confusion about the tests, how or when they’re used.
The most reliable and authorised by most governments around the world so far is PCR (polymerase chain reaction) test, which is mostly done in a lab by a trained staff. In the UAE, this test is widely available.
In other countries, it’s a different story: There’s an issue of cost, shortages of lab capacity and reagents.
Here, we describe the cheaper rapid tests and their relevance to us as we all learn to live — and deal — with SARS-CoV-2 going forward:
Q: What are the types of "rapid" tests for COVID-19?
In general, there are two types of rapid testing for COVID-19:
1. Antigen test
Detects of viral proteins (antigens) from the COVID-19 virus in respiratory samples (e.g. sputum, throat swab); and
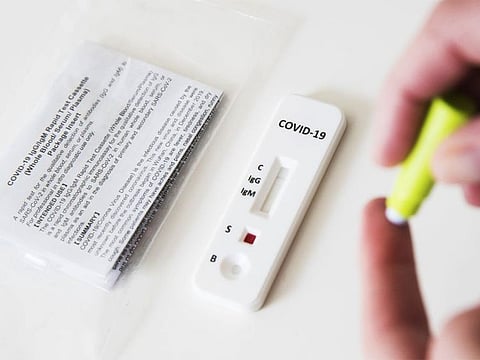
2. Antibody test
Detects of human antibodies in blood or serum (clear part of blood, free from red cells) generated in response to COVID-19 infection.
Numerous diagnostic test manufacturers have developed and begun selling “rapid” and easy-to-use devices to facilitate testing outside the lab.
They're called "rapid" because the test is usually done within minutes and at the point-of-care, at home, bedside or workplace.
ANTIGENS VS ANTIBODIES
Antibodies, also called immunoglobulins, are Y-shaped molecules — proteins naturally produced by the body that help fight against foreign substances called antigens. Antigens are any substance that stimulates the immune system to produce antibodies. Antigens can be bacteria, viruses, or fungi that cause infection and disease.
How does the antigen test work?
A typical antigen test detects the presence of viral proteins expressed by the COVID-19 virus in a sample from the respiratory tract of a person (usually via a nasal or throat swab to get a fluid sample).
Antigen tests can produce results in minutes and less expensive than molecular tests. Some experts consider antigen tests more practical to use for large numbers of people.
If the target antigen is present in sufficient concentrations in the sample, it will bind to specific antibodies fixed to a paper strip enclosed in a plastic casing and generate a visually detectable signal, typically within a few minutes.
The antigen(s) detected are expressed only when the virus is actively replicating. The WHO said such tests are best used to identify acute or early infection.
False positive and false negative?
A positive antigen test result is usually considered highly accurate.
However, there's an increased chance of "false negative" results: You have have been already infected with the virus but have negative antigen test results.
Thefore, antigen tests are not as "sensitive" as molecular tests (i.e. PCR test) are.
PREDICTIVE VALUES
Every test returns some false positive and false negative results. Tests are described by their Positive and Negative Predictive values (PPV and NPV). These measures are calculated using a test's sensitivity, its specificity, and using an assumption about the percentage of individuals in the population who have antibodies to SARS-CoV-2 (which is called "prevalence" in these calculations). How likely it is that a person who receives a positive result from a test truly does have antibodies to SARS-CoV-2? Or how likely it is that a person who receives a negative result from a test truly does not have antibodies to SARS-CoV-2? The answers depend on these measures.
Finger prick or blood from vein or swab?
The commercial tests often use a finger-prick of blood and reveal a “yes/no” answer, like a pregnancy test. The antigen test uses a nasopharyngeal swab, which gets liquid samples from the throat or nose. The molecular (PCR) test also gets a nasopharyngeal swab.
Antibody test vs PCR test: What’s the difference?
A virus like the SARS-CoV2, enters human cells and hijacks their machinery to make more copies of itself. This fires up our immune system to make antibodies to track down and kill these clones.
An antibody test checks whether you had COVID-19 in the past and now have antibodies against the virus.
On the other hand, the PCR molecular test to diagnose COVID-19. It can tell if someone is currently infected with a high degree of accuracy.
Experts say that while millions of people worldwide have been diagnosed with COVID-19, they hypothesize many more may have had it but were not tested — or didn’t even notice the infection.
What are antibodies?
Antibodies (called Immunoglobulin M, or IgM) help identify recent infections.
Some antibodies are made early in an infection and go away, usually within a few weeks, while others can linger for months — or even years.
Immunoglobulin G, or IgG, stays around longer. So far, all of the announced tests look for IgG.
A third antibody, Immunoglobulin A, or IgA, plays a role in the immune function of mucous membranes.
Antibody test vs serology test: What’s the difference?
They’re the same. An antibody test is also known as serology (blood) test. It checks for the presence of antibodies in your blood when your body responds to a specific infection, like COVID-19.
Simply put, it detects your body's immune response to the infection caused by a pathogen (disease-causing agent). It does not detect the specific pathogen (or specific virus) itself.
What’s a C-reactive protein (CRP) test?
Patients that come to clinics/hospitals with fever and other suspected symptoms may be first checked with C-reactive protein (CRP) test and whole blood cell count. These routine tests help to identify a common cold from this more severe new virus infection.
CRP is a key marker needed to diagnose and follow up the treatment of COVID-19. Chest imaging and nucleic acid test are also used to confirm the infection.
During the treatment of an infected patient, CRP is also monitored together with other biochemical markers throughout the whole treatment and recovery process.
What is a multi-protein test?
The ugly-looking COVID-19 “spikes”, which help them enter human cells, are made up of proteins, or “exo-proteins”. A protein test detects the presence of such proteins in people’s blood.
In fact, scientists have found 27 key proteins in blood samples of COVID-19 patients.
The proteins are present in different levels in COVID-19 patients, depending on the severity of their symptoms, said scientists at Britain's Francis Crick Institute and Germany's Charite Universitaetsmedizin Berlin.
This, they said, could act as predictive markers for how ill a patient could become with the disease, according to a study published by British and German scientists in the journal Cell Systems early this month (June 2020).
Three of the key proteins they found were linked with interleukin IL-6, a protein known to cause inflammation. It is also a key marker for severe COVID-19 symptoms.
What could this discovery mean for COVID-19 testing?
This discovery could lead to the development of a test that would help medical professionals predict how ill a patient might get when infected with the new SARS-CoV-2 coronavirus.
This could also provide new targets for the development of potential treatments for the disease.
It appears that those infected with SARS-CoV-2, respond differently — with some developing no symptoms at all, while others need to be hospitalised and others suffer fatal infection.
“A test to help doctors predict whether a COVID-19 patient is likely to become critical or not would be invaluable," said Christoph Messner, an expert in molecular biology at the Crick Institute who co-led the research.
This type of mutiple-protein test for COVID-19 may become available in the near future.
How long does it take for antibody test to yield results; how much does it cost?
Typically under 20 minutes. Cellex’s test, one of those approved by the US FDA, takes about 15-20 minutes.
Abbott’s test can be analysed on their machines. Each machine can run 100-200 tests a day at a cost of about $6 each, according to a company spokesperson.
When is an antibody test to be used — and not used?
In the early days of an infection when the body's immune response is still building, antibodies may not be detected. This limits the test's effectiveness for diagnosing COVID-19.
This is one reason why serology tests cannot be used as the sole basis to diagnose COVID-19.
On the other hand, testing for antibodies reveals whether a person has been infected — even if they never felt sick.
And this is where an antibody test can be useful: In the short term, it can help you answer the question: “Was I infected?”
What are the authorised antibody test kits? How much?
The US Food and Drug Administration (FDA) has authorised and verified certain antibody tests. However, many cheap $3 antibody “test kits” with questionable accuracy are now on the market.
Here’s the list of FDA-licensed antibody test kits, under the agency's emergency use authorisation scheme.
The World Health Organistion (WHO) has also outlined studies being conducted to answer questions on the optimal or appropriate use of an antibody test, as well as others.
Studies will also answer questions about the duration of immunity. The jury is still out on this immunity duration question.
SENSIVITY VS SPECIFICITY
One performance indicator of a test’s effectiveness describes its “sensitivity”, or the ability to identify those with antibodies to SARS-CoV-2 (true positive rate). The other is “specificity,” or the ability to identify those without antibodies to SARS-CoV-2 (true negative rate).
A key benefit of accurate antibody testing is that people who've recovered from COVID-19 may be eligible to donate plasma. This could be used to treat others with severe disease and boost the ability to fight the virus. Doctors call this convalescent plasma.
Why do antibody tests hold the key to vaccine development?
There are several ways antibody tests can help us all today:
1. Test volunteers in Phase III trials:
One of best use cases for an antibody test for COVID-19 is for testing those who had been given vaccine candidates.
An antibody test will help determine the success of a vaccine in Phase III trials, done on a big number of volunteers, say experts.
It will help identify individuals who may have developed an immune response to SARS-CoV-2.
2. Identify blood plasma donors:
Antibody test results can aid in determining who may donate a part of their blood (plasma), seem as a possible treatment for those who are seriously ill from COVID-19.
3. Know the extent of infection:
Because the test kits are generally affordable, Dr Marc Lipsitch, an infectious disease epidemiologist at Harvard, proposed the use of antibody tests to determine how many people have the disease and how many have immunity against it.
This is one tool that could then help policymakers decide when it’s safe to loosen social distancing rules and when they will need to tighten up again to cope with a new wave of infections.
HERD IMMUNITY
"Herd immunity" occurs when a large portion of a community (the herd) becomes immune to a disease. This condition makes the spread of disease from person to person unlikely. As a result, the whole community becomes protected — not just those who are immune. Source: Mayo Clinic [https://mayocl.in/3gfzpKG]
SPANISH EXPERIENCE
Early in May 2020, Spain published the results of a country-wide “seroprevalence” survey. It tested 60,000 residents for antibodies. The survey estimated that about 5 percent of the country’s population had been exposed to the virus, varying from 1.1 percent to 14.2 percent between regions of the country.
The survey results has several implications:
One, it means almost all of the population is still at risk.
Two, the results point to 2.3 million of Spain’s 45 million population being affected by the virus, even if they have no symptoms in many cases, considerably more than the official count of under 250,000 cases (as of June 27, 2020).
Three, data suggest there’s still no herd immunity in Spain.
Until recently, scientists have assailed seroprevalence surveys for anti–SARS-CoV-2 antibodies: the accuracy of tests posed problems, and kicked up “misleading results.” The Spanish, however, survey was lauded for the successful test and design.
Chris Sempos, an epidemiologist with the US National Institutes of Health based on the accuracy of the tests, it’s possible that the true prevalence of SARS-CoV-2 exposure in Spain is around 6 percent instead of 5 percent.
Sempos recently published a preprint version of a study showing how data from serology tests can be analyzed to produce the most accurate estimates.
“Everyone’s trying to do a good job, and they don’t have much time right now,” Sempos told The Scientist.









