How fully functional stem cell-derived pancreatic beta cells can change diabetes treatment
Research conducted by Finland's MetaStem offers possibilities for new diabetes therapies
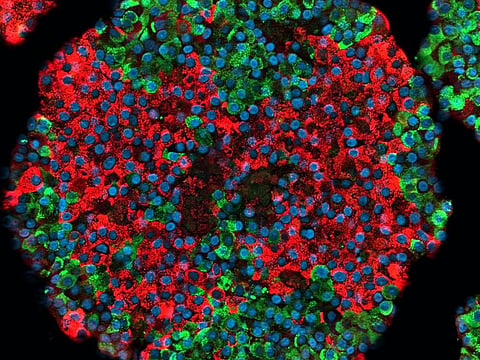
A team of researchers at the University of Helsinki, Finland has shown that it is possible to produce fully functional pancreatic beta cells that secrete insulin from stem cells, offering hope to people with type 1 diabetes.
Speaking exclusively to GN Focus, Prof. Timo Otonkoski, who led the research says the real-world applications of this finding is manifold. “This is relevant for diabetes because it gives us the possibility to study a lot of questions: what is the exact molecular mechanism in the insulin-producing cell that leads to diabetes, and then to use this information to find new drugs for diabetes,” he explains. “And of course these insulin-producing cells that we produce from stem cells could also be used for transplantation to provide insulin.”
Prof. Otonkoski is Director of Stem Cells and Metabolism Research Programme at University of Helsinki and Professor of Medical Stem Cell Research at Children’s Hospital and Biomedicum Stem Cell Center. He and his team worked under the aegis of MetaStem, the Academy of Finland-funded Centre of Excellence in Stem Cell Metabolism, which brings together experts in various fields for the study of stem cells and how their functions can be modified through tweaked metabolism processes.
Prof. Otonkoski’s team, said a press release, showcased the function of stem cell-derived pancreatic beta cells in cell cultures and later in mice studies. Once introduced to the rodents, these cells effectively managed glucose metabolism in their systems. “Blood glucose levels are higher in mice than in humans, roughly 8-10 millimolar. After the cell transplantation, the level decreased to that seen in humans, roughly 4-5 millimolar. It remained at this level, proving that the stem cell-derived transplant was capable of regulating blood glucose levels in mice,” Jonna Saarimäki-Vire, who was responsible for the cell transplantation, was quoted as saying.
Prof. Otonkoski, whose study was published in the science journal, Nature, explains that treatments derived from these findings would benefit patients with type 1 diabetes, where the body destroys its insulin-producing cells, more than those with type 2. “This is not the treatment for the common type 2 diabetes, where a person is obese and requires a lot of insulin.”
He stresses that more than cell transplantation the research would lead to important discoveries: “Our stem cell system allows us to create the model systems that will help to use patient cells to study the mechanisms of disease and then to find new types of drug treatments.”
He references another discovery made by his team, also published in the journal Nature earlier this year, which identifies the gene responsible for type 1 diabetes, TYK2. “We found with our model system that it is a very good target, possibly for the prevention of type 1 diabetes,” he explains. “We developed a system where we could study its importance and role in the insulin-producing cell. What we show is that if we inhibit the activity of this gene, we can protect the beta cells very efficiently, which are the insulin-producing cells. And the drug that is used for this purpose is already accepted for treatment in humans for psoriasis disease.”
There are therefore studies now planned to explore a new line of treatment for those with type 1 diabetes.
The journey to these discoveries, says Prof. Otonkoski, has been a long one. “I have been involved with the same area throughout my career: I started in the early 80s, studying the development of the beta cells and the possibility of using foetal cells and immature cells for transplantation. Over the years, and gradually, the research has just become more and more efficient. And now with the development of human-induced pluripotent stem cells, and embryonic stem cells, which is what we use…it’s become even more efficient.”
Many groups around the world have been working on similar research. “The only high-quality data that this crowd is dealing with these days comes from so-called pluripotent stem cells,” Prof. Otonkoski adds. Thus, the cells used for research are either human embryonic stem cells, which are cells derived from human embryos that have been donated for research, or IPS cells, which are similar to these embryonic cells, just extracted from skin or blood and genetically reprogrammed. “This is something that many groups around the world have been developing for the past 20 years or so, and definitely, our work is not very different from any other groups’ work, but now we have produced this very extensive characterisation of the cells, including insulin secretion and metabolism in comparison with adult beta cells, and that is a valuable resource for this field. So it’s not just a promise that perhaps it’s possible; we really showed that it is possible to create these fully functional beta cells.
“I don’t want to claim that it’s absolutely perfect yet. There is still work that remains to be done. But, now we are in a place where we can use these primitive stem cells to produce something that we can say is equivalent and compatible with the real thing, that is the cells that we have in our body,” he says.
The research, imperative though it is, wouldn’t be possible without MetaStem, says the professor. “These high-quality results we have produced have been possible because we could combine the excellent basic research that have been developed to study the metabolism of cells. It’s very important that there are these type of research consortiums that are putting together the expertise of the basic researchers and the clinical researchers and we are benefiting from that.”



