Aid efforts can make a difference
There is cause for tentative optimism at the new treatment centres in Liberia
Until last month, sick people hoping to get into Liberia’s overstretched Ebola treatment clinics knew there was one thing in their favour — not that it brought much comfort. Thanks to the virus’s fearfully high fatality rate, with up to seven out of 10 patients dying, ward space was always freed up sooner than later; “bed blockers” were one problem that staff did not have to worry about.
Today, it is all rather different. At the main Medecins Sans Frontieres (MSF) clinic in the capital Monrovia, a facility built for 250 people now has only around 60 patients. Further north in Foya, a forest-bound area that has been among the worst-hit, a 150-bed treatment clinic run by a different organisation was empty last week. It could not be more different from when I visited Liberia in September: MSF staff members in Monrovia were turning away up to 30 people a day, leaving some of them dying outside.
Even for an aid agency used to working in the toughest of conditions, it was a morale-sapping experience, as Stefan Liljegren, the clinic’s field coordinator, made clear. “How much worse will it get?” he said. “I have no idea.” Now, though, it seems we may have some idea — and that at last there may be signs of a breakthrough, or at least progress of a sort. The World Health Organisation (WHO), after months of grim warnings, last week confirmed a decline in the virus’s spread in Liberia, the worst-affected country so far.
And on Wednesday, it dramatically reduced its estimate of the fatalities in Sierra Leone, saying it was nearer 1,000 rather than 1,500.
What this demonstrates is the paucity of reliable data in countries where the health service has been all but paralysed by the virus, and where there are no real figures, only educated guesswork. The new WHO figures are simply a revised set of estimates and as such must be treated with caution. But even so, most health officials now believe there are grounds for tentative optimism.
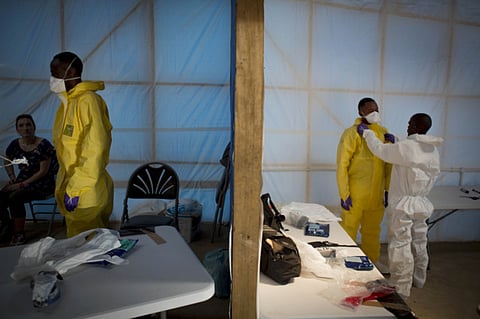
Thanks to the massive international aid effort led by Britain and America, large numbers of new treatment centres are now being built in Sierra Leone and Liberia. Meanwhile, intensive public health campaigns have finally convinced people that Ebola is not a judgement from God, a witch doctor’s curse or simply a disease that does not exist.
The virus itself, sadly, has been the most formidable public educator of all — after nearly 5,000 deaths across West Africa, far fewer people now ignore the rules about touching bodies at funerals or shaking hands.
None the less, while staff at the MSF clinic in Monrovia are no longer overwhelmed, few expect to pack up their makeshift clinic’s rows of white tents any time soon. Natasha Reyes, the charity’s medical coordinator in Liberia, said there may have been “a behavioural change”, but she believed that some Ebola sufferers may simply be choosing to die in company at home rather than alone in an isolation clinic.
“It is too early to make any real conclusions,” she insisted.
So when might we be able to? Epidemiologists are focused not on a timeline, but on a particular formula called the Reproductive Ratio. Known as R0, or “R-nought”, this is a basic measure of Ebola’s infectiousness. Its current value is between 1.7 and 2.0, which means that every 10 people who become infected will pass the virus on to another 17-20 people before they either die or fight the virus off. If 70 per cent of infected patients can be put in clinical isolation — a figure that may be possible given American and British-led efforts — that ratio will hopefully diminish to less than 1.0, at which point the number of new cases for every set of existing ones should start to fall. By that criteria, the epidemic could be over by late January, according to America’s Centres for Disease Control and Prevention.
And should that welcome moment come, there will no doubt be those who conclude that this has been yet another global health scare in the manner of the South Asian Respiratory Syndrome (Sars) virus, for which the £225 million (Dh1.3 billion) that Britain has committed to Sierra Leone is yet another example of a bottomless aid budget.
However, bear in mind that international disease epidemics are not cost or resource-predictable beasts. Arguably, the only appropriate level of response is the one that stops it in its tracks.
Besides, even if West Africa is eventually given the Ebola all-clear, it has effectively spent six months in an economic and political coma. Quite apart from the psychological impact of suffering a modern-day equivalent of the Bubonic Plague, government services have all but collapsed, schools have been shut and businesses forced to the wall.
The patient may pull through, but the period of convalescence is likely to be long and painful.
Sign up for the Daily Briefing
Get the latest news and updates straight to your inbox


