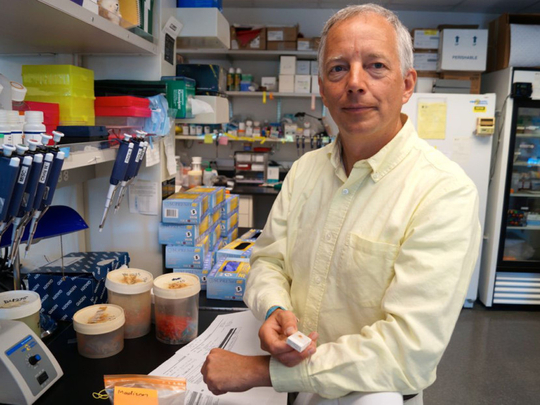
Jim Olson is a paediatric oncologist whose research is being talked about around the world thanks to some innovative thinking — and scorpions. Based at the Fred Hutchinson Cancer Research Center in Seattle, he leads a team whose biggest success is “tumour paint”, a drug that attaches to cancer cells, lighting them up so it is easier for surgeons to operate successfully.
The paint was developed from chlorotoxin found in scorpion venom and is being tested in clinical trials at present. So excited was Olson, 52, by this discovery that he had the knot of bonds at the centre of the chlorotoxin molecule tattooed on his upper arm. Decorating his office are framed photographs of his patients at Seattle Children’s Hospital, who are clearly the motivation for his work: he is driven by a desire to tell more parents their children will survive.
His quiet, unassuming manner belies the passion and energy with which Olson approaches life — both at work and in his leisure time when he cooks, cycles and kayaks with gusto. He remains close to many of the families he meets and is a tireless campaigner, successfully using social media and crowdfunding to publicise and raise money for his research.
Your biggest success is “tumour paint”, which makes cancer cells easier to spot during brain surgery and is now in five human trials. How was this developed?
We had a patient who had brain tumour surgery in 2004, which left much of her tumour behind because the surgeon thought it was normal brain and didn’t want to paralyse her. When we realised how much was left behind and the problem for the surgeon not being able to easily distinguish cancer from normal brain, we committed to developing a technology that would light up the cancer.
We focused on the scorpion toxin chlorotoxin, because what was thought to be the target of that molecule was present on brain tumour cells but not on brain cells. I figured that if there was ever a creature that could get a molecule into the brain, it would be the scorpion because they need to paralyse their prey.
So we grew a human tumour on the back of a mouse; we connected the toxin (from the deathstalker scorpion) to a fluorescent tag and injected it into the mouse, and a couple of hours later the cancer was brightly glowing. It was a very exciting day.
As well as lighting them up, can this scorpion molecule also deliver chemotherapy drugs to tumours?
This wouldn’t be the right molecule to do that because a fair amount of it also goes to the liver and the spleen. If we put a toxin on it, it would also wipe out those normal organs. Through our current research we’ve identified a different molecule from a different organism — a grasshopper — that goes to cancer but much less to the liver and spleen. That’s the foundation for our future work.
Does tumour paint work for other cancers?
In prior work, the tumour paint molecule, known as BLZ-100, lit up a variety of cancers in dogs. Now scientists at Blaze Bioscience (the spin-off company co-founded by Olson which is running the ongoing human clinical trials) have reported that in skin cancer patients, the BLZ-100 signal was present in nearly all cases of confirmed cancer and was absent in most cases where the pathologist determined that the skin lesion was not cancer.
What is the difference between tumour paint and fluorescent imaging with 5-ALA that is approved for use in Europe but not the United States?
With 5-ALA surgeons can often get a better resection and patients a better outcome than without it. It does have some limitations. When there’s a brain tumour and the blood-brain barrier (which keeps nasty things out of our brain) is disrupted, the 5-ALA will get in there and light up that area.
The challenge is that sometimes there are parts of the tumour where the blood-brain barrier is not interrupted, it’s intact, and so those don’t light up with 5-ALA.
We set out to find a molecule that crosses the blood-brain barrier so it could light up tumours either way, whether the blood-brain barrier is intact or not, and where the drug actually binds to each cancer cell and goes inside the cancer cell and makes them glow so that surgeons can see cell by cell. We hope it will be much more accurate.
What drives your work?
Each week when I go to clinic, I ask myself: “What are we going to do today that I don’t want to be doing in 20 years, and how can my lab play a role in changing that?”
Why did you decide to go into paediatric oncology?
I took care of a little girl who passed away. Her parents told me that my words with them made her death as beautiful as her birth and that through the conversations we’d had, they’d learnt that a life could be seven years long or 70 years long and what mattered was the beauty of what occurred during that time. I thought I had something to offer when the medicine didn’t go the way you wanted it to.
There are many photographs of children you have cared for in your office. How do you cope with the emotional side of your work?
I realised early on that I was going to suffer and be in pain when these kids passed away or weren’t doing well whether I chose to compartmentalise it or not. I decided to go all in and fully love each child and each family and to become part of that family the day we meet. You can take extraordinary ups and downs when you are part of a family. I stay close to many of them.
Do you have children?
I’ve got two daughters, 21 and 17. They are both wonderful writers, activists and feminists. My older daughter is head of the animal rights group at the University of Washington so you’d think there’d be a big clash, but she did a TEDx talk last year and she wove our work together.
My team tries to minimise the use of animals and importantly we’re very open to using alternatives when the alternatives are useful and accessible. Her point is that similar investments should be put into finding alternatives to animal testing as to continuing the status quo. We have very good and respectful conversations.
Is it frustrating that it takes so long to bring a new drug to market?
Well, it is — take tumour paint as an example. My own mother had a cancer that would definitely have benefited from it and it was too early to use it. It started in the skin on her face and went back into her brain. It ended up spreading extensively and that could have been avoided if it had been understood that they hadn’t got it all and had gone a little bit deeper.
She’s doing fine now, two years later. I love my patients in the same way, so every week when we have kids, and we can’t use it yet ... These things just take time though.
The reality is that if things move forward too fast you can have really serious safety problems. I don’t get frustrated because frustration doesn’t help you move forward.
How do you fund your research?
Most innovative ideas are really hard to get approved through peer review (and therefore funded by grants) ... so the families stepped up by doing chilli cook-offs, golf tournaments and auctions and they’ve raised over $10 million (Dh36.7 million) since the late 1990s. In 2013 we launched Project Violet. We’re well past $5 million with that.
Tell us about Project Violet.
We decided to build a platform where we could identify other similar molecules (to the tumour paint molecule) that plants and animals use for protection in nature, and find a way to create hundreds of thousands of variations of these that could be used for screening for human diseases.
I realised that to do this we were going to need to build a team of experts. We launched Project Violet so we could use social media and the public domain to cooperatively build these libraries of drug candidates. I launched that in my TEDx talk in June 2013 and since then we’ve been able to support, or partially support, 33 scientists. For a year around that, volunteers from Amazon in Seattle helped us build our website and our social media presence.
Violet was a little girl who had a type of brain tumour that I’ve not yet had a child survive. She knew she was going to die. She decided to donate her tissue when she died to help other children. Also, some of these molecules we’re working on come from the violet plant.
Any other research successes?
One day, I realised I was prescribing medicines with no idea whether the cancer would be resistant to that drug. So, I hired two bioengineers and we created a technology where needles are exerted through the skin into a tumour and as the needles are withdrawn they leave behind tracks of different drugs. You let those drugs be present around the tumour cells a day or so, then take out the tumour and cut across-wise to the needles and see which ones work and which don’t.
If a drug doesn’t kill any cancer cells when they are bathed in it, it certainly isn’t going to get any better when you give that drug as an IV or by mouth. I think this is going to revolutionise cancer and drug development.
–Guardian News & Media Ltd













