Leave it to the youngest person in the lab to think of the Big Idea.
Xuyu Qian, 23, a third-year graduate student at Johns Hopkins, was chatting in late January with Hongjun Song, a neurologist.
Song was wondering how to test their three-dimensional model of a brain — well, not a brain, exactly, but an “organoid”, essentially a tiny ball of brain cells, grown from stem cells and mimicking early brain development.
“We need a disease,” Song said.
Qian tossed out something he’d seen in the headlines: “Why don’t we check out this Zika virus?”
Within a few weeks — a nanosecond compared with typical scientific research time — that suggestion led to one of the most significant findings in efforts to answer a central question: how does the Zika virus cause brain damage, including the abnormally small heads in babies born to infected mothers?
The answer could spur discoveries to prevent such devastating neurological problems. And time is of the essence. One year after the virus was first confirmed in Latin America, with the raging crisis likely to reach the United States this summer, no treatment or vaccine exists.
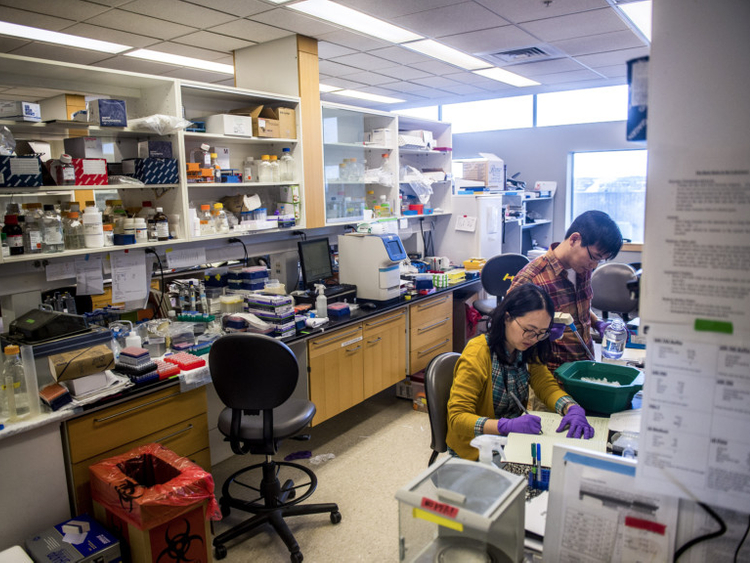
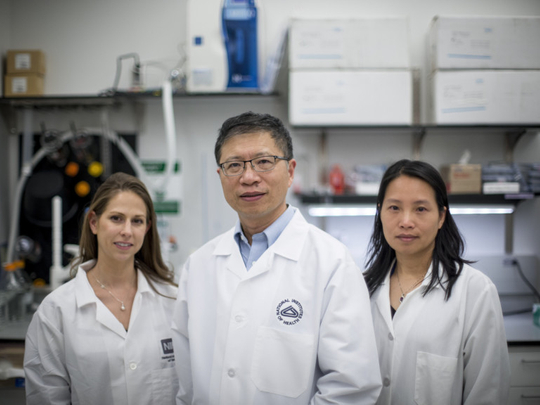
“We can’t wait,” said Song, at the university’s Institute for Cell Engineering, where he and his wife and research partner, Dr Guo-Li Ming, provided a pipette-and-petri-dish-level tour. “To translate our work for the clinic, to the public, normally it takes years. This is a case where we can make a difference right away.”
The laboratory’s initial breakthrough, published in March with researchers at two other universities, showed that the Zika virus attacked and killed so-called neural progenitor cells, which form early in foetal development and generate neurons in the brain.
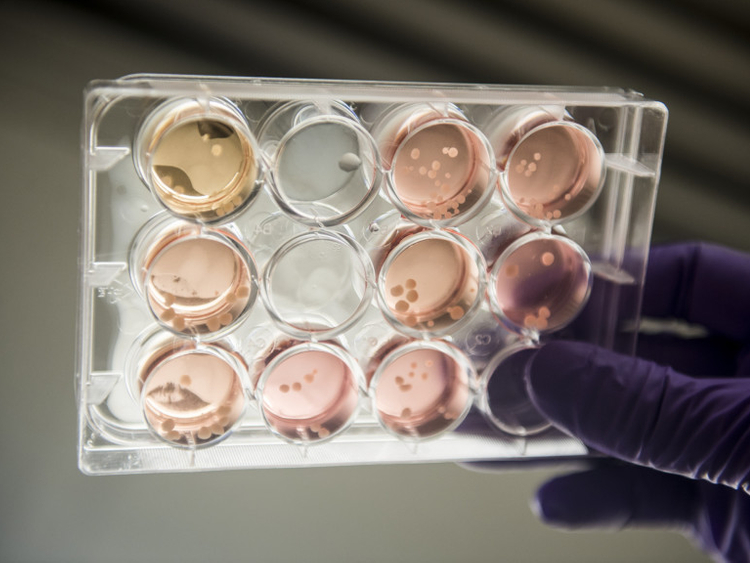
In April, the team and other collaborators published a study in the journal “Cell” showing that this assault by Zika resulted in undersize brain organoids: damaged progenitor cells created fewer neurons, leading to less brain volume.
That may explain the smaller brains and heads, a condition called microcephaly, of some babies exposed to Zika during pregnancy.
“I think they’ve nailed it,” said Dr Eric Rubin, a professor of immunology and infectious diseases at Harvard. “That is totally consistent with the pathology that has been seen in the children that died or the aborted foetuses.”
The experiments here suggest other worrisome aspects of Zika infection: that even low doses of the virus for short periods can cause damage and that it is most dangerous in the first trimester of pregnancy but can also be harmful in the second.
“The really sad news is not only can the virus infect neural progenitor cells, but it turns them into a factory,” Song said.
“The cells produce more virus and they actually can spread it,” said Ming, adding that infected cells appear to create a “bystander effect”, releasing chemicals as they die that damage or kill neighbouring uninfected progenitor cells.
And the organoid results contain a frightening hint of why Zika is also associated with adult neurological disorders, including Guillain-Barré syndrome, a temporary paralysis. Song said they found that Zika infection is “even worse” in glial cells, which support and insulate neurons and are present throughout life, not just in foetal development.
But there is much more to learn, and the collaboration catalysed by a remark from a junior scientist now includes nine labs at six sites across the country.
Among them is a specialised lab at the National Center for Advancing Translational Sciences, which is testing drugs on neural progenitor cells, hoping to find compounds that can stop the virus. Rapidly testing thousands of compounds in varying doses, the lab has already zeroed in on a promising candidate. If the drug succeeds in further testing, it could allow scientists to skip much of the safety evaluation necessary for creating new drugs or vaccines.
Many other researchers are also rushing to understand how Zika wreaks its damage. Teams in Brazil and at the University of California, San Diego, have also found that the virus attacked neural progenitor cells and shrank brain organoids. The San Diego team reported that Zika overactivated a molecule that normally protects against viruses, and the excess activity seems to switch on genes that galvanise progenitor cell destruction.
A rush of research
In Rio de Janeiro, Stevens Rehen, a neuroscientist at D’Or Institute for Research and Education, said the Brazilian team was also testing drugs, seeking one that blocked the Zika virus. But they can test only those approved in Brazil; importing drugs from elsewhere involves weeks of red tape. “The idea is to be fast,” Rehen said.
At the University of Pittsburgh, Carolyn Coyne, a microbiologist, and Dr Yoel Sadovsky, an obstetrician and microbiologist, are investigating how the virus enters the placenta. They determined that Zika does not infect trophoblasts, placental cells that protect against most viruses.
But there could be other routes: does the virus sneak in through breaks in the lining? Does it hide in “Trojan horse” cells? Does it piggyback on antibodies from related infections, such as dengue?
“Going through the placenta is not the only way to infect a foetus,” Sadovsky said.
Separately, scientists at other institutions, including Vanderbilt; the University of California, San Francisco; and Washington University in St Louis, are examining questions such as how the immune system recognises the virus.
Experiments from all these labs will provide clues, Rubin said. But they will not tell the whole story. “In a person, it’s way more complicated,” he said.
Song and Ming, both 46, met as high school classmates in Wuhan, China. Now at the Institute for Cell Engineering, their offices are both on the seventh floor. “She has the better view,” Song said.
Their son Max, 17, is an adjunct lab member of sorts, and his artwork mapping the Zika virus’s international journey graces the cover of the journal that published his parents’ first Zika study, “Cell Stem Cell”.
By February, the couple was puzzling over how to study the Zika virus when they had no samples of it; even if they could get some, their lab did not have university approval to work with Zika.
Then Song received an e-mail from his friend Hengli Tang, a virologist at Florida State University. Since meeting as graduate students, they had vacationed and celebrated holidays together, but never worked together.
He e-mailed Song. Seconds later, the phone rang.
“He said, ‘I didn’t read the e-mail, I just saw Zika and called’,” Tang recalled. “He was all excited and said, ‘We were just discussing where to find Zika, because we have the perfect system to study Zika’.”
The next day, neural cells were winging their way to Tang’s lab in Florida, packed in vials in ice, the first of many rapid-fire FedEx exchanges. (At one point, FedEx temporarily interrupted the breakneck pace by delaying a shipment, questioning whether the unit of measurement, millilitres, was correct, Tang said.) The Johns Hopkins researchers sent four kinds of cells: two types of stem cells, which can be turned into other human cell types; neurons; and neural progenitor cells.
A scramble for samples
Song and Ming were betting the Zika virus targeted neural progenitor cells; they had long studied microcephaly cases unrelated to the Zika virus and knew progenitor cells were damaged in those cases.
They sent cells derived from two people, one healthy and one with schizophrenia, because those were the cells they had, and they wondered if schizophrenia would yield different results. It didn’t.
It takes years to learn to handle these finicky cells. Tang had no such experience, so a Johns Hopkins postdoctoral student, Zhexing Wen, immediately flew to Florida to help. Later, Xuyu Qian did, too.
Because the students in his lab are young women, Tang opted for safe-handling precautions beyond those normally required for Zika.
He was not expecting much from the first experiments adding Zika to the four types of cells. “To be honest, this was supposed to be a pilot study,” he said. “We had no idea whether, first of all, the virus would even infect these cells.”
But within a week, the results were striking. The virus attacked neural progenitor cells much more aggressively than the neurons or stem cells.
“I was overwhelmed,” Song said.
Suddenly they had a likely answer to “one of the very first questions people want to know”, Tang said.
The results suggested that the Zika virus was most dangerous in the first trimester, when most progenitor cells form. In those cells, the infection increased activity of an enzyme, caspase-3, which signals and also contributes to the death of cells, Ming said.
In healthy humans, this and other enzymes contribute to “programmed cell death”, necessary so cells do not divide or grow endlessly, like cancerous cells. But kill too many cells or at the wrong time, and development goes awry, drastically.
Quickly, the Johns Hopkins researchers found their cellphones buzzing as other scientists saw ways to build on their results.
“There’s so many e-mails I can’t keep track,” Song said. “It’s, ‘I’m missing this piece, can you send me that?’ or ‘I don’t understand this part’.”
But the first experiments lacked a crucial element, they knew. They were done on cells in plates, in 2D. How would Zika work in 3D, in a more complex, more brainlike experiment?
Enter the brain organoids, spheres at most the size of a BB, containing stem cells differentiated into most types of brain cells. As they grow, they mimic foetal brain development; a 100-day-old organoid resembles the late second trimester of pregnancy, Ming said.
They shipped organoids to Tang in Florida, a task made easier because three high school students, including Max, had spent summer internships designing miniature spinning bioreactors, used to incubate organoids. Constructed with 3-D printed parts, they were smaller than standard bioreactors and cheaper to use because they needed less cell-growing material.
Meanwhile, after the March finding, the NCATS lab in Rockville, Maryland, sprang into action. Wei Zheng, who runs the lab, part of the Therapeutics for Rare and Neglected Diseases programme, said the fact that Zika increased the caspase-3 enzyme gave him a way to test drugs on cells infected with Zika.
First, search for drugs that block the spike in caspase-3. Then, weed out those drugs that are toxic to the cells themselves. Finally, see if any remaining drugs prevented the Zika virus from killing cells.
Zheng noted that Zika took about three days to kill its progenitor cell victims, and did not kill all of them. If it did, he said, “you wouldn’t see a baby” at all.
It is possible, though, Ming said, when Zika strikes very early in pregnancy, it destroys so many cells that miscarriage results.
A possible testing gold mine
NCATS has perhaps the world’s largest collection of drugs and compounds, some half a million. During a recent visit, an employee who goes by the name Pepper showed how samples are fetched from glass-walled carousels by giant yellow robotic arms in a meticulously programmed ballet resembling an albatross love dance.
Many of the compounds are untested in people. But one collection contains about 2,800 drugs approved in the United States or other countries. Another library holds about 2,000 compounds that have been through some human safety testing.
The Johns Hopkins researchers needed time to grow more neural progenitor cells, but Zheng started anyway, first on brain tumour cells he infected with Zika. Three compounds seemed effective — a caspase inhibitor, a Russian antidepressant, and a common vitamin — so he whisked them to other researchers to try.
After receiving progenitor cells, he started again. He found 173 drugs blocked caspase-3 increase, about three dozen did so without harming cells, and one — just one — prevented the Zika virus from killing cells. That drug, which he declined to identify, is not approved but has undergone safety testing and is in a clinical trial with cancer patients, he said.
He sent the drug to Johns Hopkins, where early testing is yielding similar results. But even if results are replicated in mice and humans, hurdles remain, including determining if it is safe for pregnant women and deciding who to treat, since many women infected with Zika have had healthy babies.
Also, a drug that can “save the cells after they’re infected” is not the real prize, Song said. “The best drug would actually prevent the cells from being infected in the first place.”
–New York Times News Service