Spotting my roots peeking through, I got out my black hair dye. Having coloured my own hair since I was 16, I knew the routine. But 20 minutes after blow-drying, my hair was wet again. Fluid was oozing from my scalp. Shocked, I realised it must be an allergic reaction, although I’d used the same brand of hair dye many times. Along with oozing, my scalp itched then my whole body started itching.
My youngest daughter, Heather, who was aged seven, has eczema so I’d become an expert in skincare and what might trigger problems. Still, my skin’s extreme reaction was frightening. As the dye was permanent I couldn’t wash it out. So, desperate to get rid of any lingering chemicals, I rinsed and rinsed my hair and coated my scalp with eczema creams. My skin calmed down, my body stopped itching, but my hands looked as if they didn’t belong to me. The skin was so dry it itched, peeled, cracked and stung, and none of the eczema treatments I tried over the next few weeks made any difference.
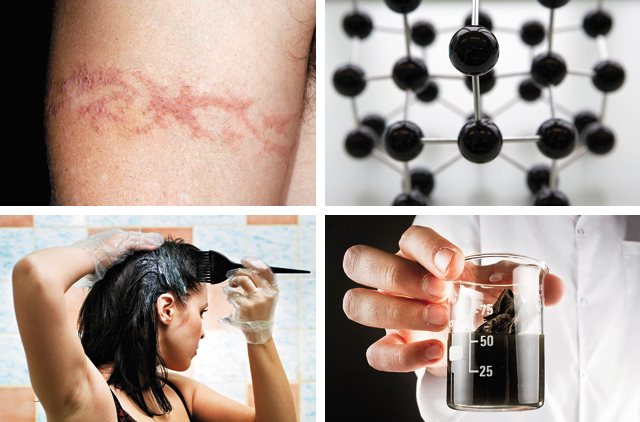
Turning detective, I found people can become allergic to PPD (paraphenylenediamine) – a chemical found in black dye. A dermatologist arranged allergy testing where, using pinpricks, they put some likely allergens into my skin to see which would cause a reaction. “Definite reaction to black dye,” he said, suggesting that I stick to PPD-free henna. “Try to eliminate any contact with black dyes,” he warned.
As he ran through a list of what would be likely to affect me – newspaper print, photocopied paper or printer ink, black clothes, black shoes and handbags – I realised I would have to ditch two-thirds of my wardrobe. After leaving his office, I sat in my car, saw the black leather steering wheel, black Filofax, black seat... I knew this would be a huge challenge.
I was prescribed emollients and steroids. Steroids work for some. I was unlucky. One brand caused the skin on my hands to go hard, like old leather, so rigid I couldn’t even bend my fingers much. Others did little.
High sensitivity
Eliminating black dye from your life is incredibly hard as it’s all around us. Even without touching dye directly, someone only needs to grab a handle after touching newsprint and enough traces of dye are left to aggravate the hands of someone like me, who’s severely allergic. Despite applying emollient creams ten to 15 times daily I woke with hands raw and bleeding from scratching in my sleep. My cracked skin repeatedly became infected.
Think of how it stings washing your hands when you have a cut. Now imagine cuts on every line in your palm. It stung so badly I couldn’t help crying out with pain when showering, and everyday chores like peeling potatoes or washing out a coffee mug became excruciating or impossible.
I tried not to let my daughter know how bad it was, as I didn’t want to upset or frighten her – but she knew without me saying anything. Instead of slipping her hand into mine as we walked along the street, she’d ask first in case it was a very bad hand day. That made me so sad. I’m a business development manager, so I have lots of meetings. I stopped shaking hands when greeting people, partly because a firm handshake would leave me wincing, but also from embarrassment as you could see people almost reel back in horror when they spotted the cracks and blistered, terrified that whatever I had was contagious.
I also had to stop rock climbing and other outdoor activities I loved because I couldn’t afford to get my hands dirty as they quickly got infected. I raged inwardly about the limits this allergy was enforcing on my life. Even changing gear in the car made me squeal. Contracting the allergy to black dye seemed to sensitise me to other allergens too, so nickel became a problem and that’s in coins, keys – all kinds of everyday metal items.
The only option was to wear cotton gloves all day, every day. These kept soothing cream in place without spreading it on to everything else and kept my hands clean, but within hours they would become soggy and fall off! They also didn’t wash well so I needed two to three new pairs a week, which became pretty costly. Wearing gloves for everything is impossible though – I couldn’t put on make-up with them, and touch screens don’t work through the gloves, so to use GPS in the car I had to take them off.
Try wearing gloves for 24 hours and you’ll see just how difficult they can make life! One night when my husband and I were attending his company’s dinner and dance I wanted to wear a slinky gold dress. I knew the gloves would utterly spoil the look, so I left them off. I also went cream-free so I wouldn’t leave greasy marks on everything and everyone I touched. It was agony. I could hardly pick up the knife and fork to eat. After a few hours I made my excuses and shot to our room to put the cream and gloves on.
Finding the solution
Luckily I could abandon the cotton gloves when I discovered silk gloves on the internet. As soon as I put those on, the itching stopped and any infections I had soon cleared (apparently the silk works like a gentle steroid). I also persuaded Dermasilk, the company that made my brand, to make fingerless versions, which were great as they protected the palms but left fingertips free so I could still put on my make-up or touch screens.
Still, despite the gloves, creams and avoiding touching anything black, my hands remained a painful mess, so you can imagine how pleased I was when nearly two years ago I read about a treatment that was starting to become available through dermatologists. Made from alitretinoin, which is chemically related to vitamin A, these capsules were called Toctino. It took months of research for me to find a dermatologist willing to prescribe it to me, as many seemed not to know anything about it.
Even when I found a sympathetic and knowledgeable dermatologist at The James Cook University Hospital in Middlesbrough I had to jump through hoops before she would prescribe it for me. You can’t take it while pregnant as it can cause birth defects, so the dermatologist did a pregnancy test just to be certain even though I’m post-menopause. My cholesterol and thyroxine levels were checked as the drug can affect those, and I had to complete a questionnaire to assess how badly hand eczema was limiting my life.
I was warned to go back if I developed any problems with my eyes, developed aching joints or hot flushes, and my liver and kidney function were checked, as the drug can affect those too. It sounded so scary, but I was absolutely desperate to have hands that worked properly and weren’t so painful, that I was prepared to take the risk. Eventually I was given a four-week course, which I started in June 2011.
Within two weeks my hands were virtually clear. I was staggered. Although I had high hopes for the treatment, this seemed almost miraculously quick. After that initial month, I took a break from the drug and the eczema came back. I then took a 12-week course, hoping that would cure it completely. Unfortunately, every time I stopped Toctino my hands deteriorated, not quite as bad as before but bad enough for me to go back on.
For over a year now I’ve been on the drug and while I had a muzzy headachey feeling for the first few days of treatment, it’s had no effect on my cholesterol or anything else that I can spot. To say I’m grateful for getting my hands – and my life – back is an understatement. I can wash my own hair, do the gardening, decorate, a million little things I couldn’t do for years. Best of all, I can now hold hands with my husband and my daughter.
Pam Patterson, 49, lives in Durham, England
Could your hair dye kill you?
Hair dye has been linked to violent allergic reactions, which have resulted in comas and even death in the case of a 17-year-old British woman, who vomited and then fatally collapsed after using a home hair-dye kit in 2011. Doctors and paramedics suspected adverse reaction to paraphenylenediamine, an organic compound used in most permanent hair dyes.
“Paraphenylenediamine (PPD) is a chemical substance that is widely used as a permanent hair dye,” says Dr Burcu Barutcuoglu Hurbas, specialist dermatologist at the American Academy of Cosmetic Surgery Hospital, Dubai Healthcare City. “It is generally colourless and only gains its colour when exposed to oxygen. It can be mixed with henna, which is often used for painting the body or in temporary tattoos. PPD derivatives can also be found in textile or fur dyes, dark-coloured cosmetics, photocopiers and printing inks.”
Common symptoms of a PPD allergy are redness, itchiness, swelling on the scalp, forehead, eyes and ears. A reaction normally occurs when the chemical comes into contact with the skin while the dye is oxidising. If you develop any of these symptoms while dyeing your hair Dr Hurbas advises washing your hair and scalp thoroughly with a mild soap or shampoo to remove the excess dye. Reactions to henna painting may be delayed for two weeks because the chemical is applied while it is in its oxidation process.
“The reaction can be quite severe, almost similar to that of a chemical burn, says Dr Zaid Jasim, a consultant dermatologist at the Dr Sulaiman Al Habib Medical Centre in Dubai. PPD allergy can also cause allergic contact dermatitis. If severe allergy occurs, it can spread all over the body and even cause anaphylaxis (swelling of the tongue and throat). Visit a dermatologist as soon as one notices the occurrence of rashes and skin reactions. Allergy from hair dyes can be diagnosed through testing on the skin behind the ear and localised redness appearing within two days confirms the diagnosis.
“Mild to moderate allergies can be treated with topical treatments only, while oral corticosteroids may be prescribed in addition to topical corticosteroid creams and ointments for severe cases,” says Dr Jasim. Very severe cases may require hospitalisation. People whose job requires them to constantly work with PPD, such as hairdressers and film developers, often develop dermatitis on their hands. A patch test usually reveals hypersensitivity to PPD. The best way to cope is to avoid contact with the allergen by wearing suitable protective garments such as gloves and protective sleeves.
If you’re allergic to PPD try to avoid the use of all oxidation hair dyes, Dr Hurbas advises. The good news is some newer permanent and semi-permanent hair dyes that use para-toluenediamine sulphate (PTDS) instead of PPD are now available at pharmacies. “These are likely to be tolerated by about 50 per cent of people who are allergic to PPD,” says Dr Hurbas. But remember that patch-testing is recommended prior to use.
Additional reporting by Khulekani Madlela