Last week, a Pakistani doctor was sentenced by his government to three decades in prison for actions that helped the United States kill Osama bin Laden. Meanwhile, in far-off Geneva, the World Health Organization (WHO) declared a state of emergency in its decades-long battle to eradicate polio. That these two events are intimately connected speaks volumes about new challenges - political ones - that threaten to undermine extraordinary global health achievements.
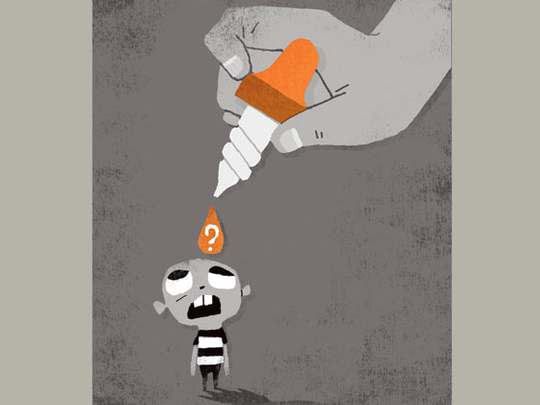
A tribal court in Peshawar sentenced Dr. Shakil Afridi to 33 years’ imprisonment for treason - a penalty considered mild given that the nontribal Pakistani government courts would have ordered death by hanging for the same alleged crime. Afridi collaborated with the CIA’s efforts to determine if the secretive family residing behind high compound walls in Abbottabad in 2011 was the bin Laden clan, as U.S. officials suspected. His role was to use a fake hepatitis-B vaccination campaign to gain access to the children in the compound, administer immunization, and retain the needles for use by CIA lab scientists to identify the youngsters’s DNA.
Bin Laden was indeed inside the compound, which was raided by U.S. Navy Seals on May 2, 2011, resulting in the death of the al Qaida leader. U.S. officials later told The New York Times that Afridi had failed to obtain the desired DNA samples, but the physician has publicly admitted to collaborating with the CIA in the vaccine ruse. A chorus of U.S. politicians and Obama administration officials have denounced Afridi’s conviction, arguing that the doctor had not acted in betrayal of his country, but in opposition to al Qaida.
This week, tribal court documents were released showing that the doctor’s ultimate “crime” was an alleged association with the militant Pakistani insurgent Mangal Bagh, a claim widely dismissed by human rights observers as false. The same day Afridi received his sentence, leaders attending the Geneva meeting of the World Health Assembly (WHA), the WHO’s governing body, declared a state of emergency in the global effort to eradicate polio. With a $1 billion shortfall and only the last 1 percent of polio to go, WHO chief Dr. Margaret Chan declared on May 24, “polio eradication is at a tipping point between success and failure. We are in emergency mode to tip it towards success - working faster and better, focusing on the areas where children are most vulnerable.”
In the 1980s, an estimated 350,000 children in 125 countries annually contracted polio; the WHO believes that this year, just 100 cases of the disease have surfaced worldwide. The end is so near that the Rotary Club, which has made eradication of polio one of its core missions, has champagne on ice. In February, the WHO declared that for 12 months India was free of polio for the first time in the known history of the massive nation, leaving just three countries in the world with endemic polio: Afghanistan, Nigeria, and Pakistan. Not coincidentally, all three have huge Muslim populations. Nigeria has struggled with polio control since 2003, when a group of imams in the country’s Islamic north declared the vaccine was deliberately contaminated with either HIV or contraceptives, the result of an alleged CIA campaign to wipe out Muslim children.
The conspiratorial view of polio control was shared by some imams and Muslim politicians in Pakistan and Afghanistan. So last July, when it was disclosed that the CIA had used Afridi and a false vaccination campaign to gain access to the Abbottabad complex, I co-authored a warning with Dr. Orin Levine that the CIA had “destroyed credibility that wasn’t its to erode.” We wrote: “It was the very trust that communities worldwide have in immunization programs that made vaccinations an appealing ruse. But intelligence officials imprudently burned bridges that took years for health workers to build.”
A year later, we have crossed a Rubicon, as WHO Assistant Director General Bruce Alyward told the World Health Assembly. Polio has been eradicated from all the world save those pockets least likely to have faith in Westerners, and the final assault on the virus is hampered by distrust that was in part sown by the CIA. Worryingly, religious leaders in Southern Sudan are reportedly now advising mothers to refuse vaccination for their babies.
The WHO, the Rotary Club, and other leaders of the anti-polio campaign have enlisted support from top Muslim religious figures around the world to counter such vaccine apprehensions and conspiratorial views. But it’s hard when the conspiracies prove true. The tragedy is that we could be on the verge of a new outbreak, just as we are on the verge of success. The continued wild-type polio circulation - the epidemiological term for various natural forms of the virus - in neighboring Pakistan and Afghanistan causes grave concern in India, where any reintroduction of the virus carried by outsiders into Indian territory could be dangerous due to under-immunization of millions of babies, now children, in pre-2010 campaigns. Even as India changed vaccination tactics and was bringing its polio caseload down to zero, incidence soared in next door Pakistan last year.
In late 2011, 10 cases of wild polio turned up in China, carried across its border from Pakistan into territory where health officials had eradicated the disease. Alarm across Asia skyrocketed. As cries of concern from New Delhi grew louder, earlier this year the WHO gave Islamabad a stern warning: Stop polio or face global health travel restrictions, which would be economically crippling. After two years of mishaps in its bungled immunization efforts, Pakistan’s health leadership went overboard, stopping cars at tollbooths and dropping polio vaccine into every child passenger’s mouth.
By April, local polio trackers sent numbers to Geneva that the WHO interpreted as hopeful signs that the disease was finally coming under control. But recently, Pakistan’s chief health commissioner Tariq Pirzada revealed that the numbers were faked by overzealous officials eager to please the WHO. In truth, rural immunization rates remain appalling. The call for polio eradication goes back decades, and was initially backed by millions of members of the Rotary Club International, which raised much of the money used to eliminate the disease from the Americas, nearly all of Africa, and Southeast Asia. More recently, philanthropist Bill Gates jumped into the fray, donating billions of dollars to the effort. Combined with the WHO, UNICEF, and other organizations, these players eliminated 99 percent of the global burden of the disease, including cases of permanent paralysis caused by the crippling virus and deaths. But in mid-May, U.N. Secretary-General Ban Ki-Moon warned that the great achievements to date could collapse if polio efforts fail in Afghanistan, Nigeria, and Pakistan. “There is a looming danger that we could fall victim to our own success,” he warned.
“Here’s why: The world is now populated by a generation that for the most part has never been exposed to polio. Additionally, many in this generation have been inadequately vaccinated. When the virus strikes under those conditions, the impact can be devastating. We saw that in the Republic of Congo and elsewhere in Africa in 2010, when an outbreak killed half of all who contracted the virus.” Eradication is tenuous. Since the early 1960s it has been known that the polio virus can be carried by higher primate species, including monkeys, chimpanzees, and gorillas. In the laboratory it is also possible to infect rodent and chicken cells with the virus, though there is no evidence of those species carrying polio in nature. Nevertheless, unlike smallpox - the only human pathogen ever eradicated - polio isn’t merely a Homo sapiens germ. The virus, moreover, enters the human body in multiple ways, and after vaccination may continue to reside in the gastrointestinal (GI) tracts of infected individuals.
Back in the 1950s, when scientists Jonas Salk and Albert Sabin competed to be the first to invent a vaccine, Salk created an injectable version that eliminated the virus from the individual’s bloodstream, built up antibodies, and completely protected children from the disease. But Sabin showed that those children could still harbor viruses (harmlessly to themselves) in their GI tracts, and shed infectious microbes in their feces. Thus, Sabin said, oral vaccination was preferable, as it cleansed the intestines and built up local cellular immunity that protected not only the vaccinated individual, but the general public health by eliminating fecal passage of virus into water supplies, food, and untreated sewage systems.
Broadly speaking, this conflict between oral versus injected vaccination, public versus individual protection, and lifelong immunity versus temporary was at the heart of ongoing technical disputes regarding how best to target the disease, and whether eradication is even possible. While oral vaccination is easier than giving shots, its immunization impact is weaker and wanes with time - even fairly recently immunized Indian children are showing signs of lost protection. Overcoming this requires giving a child as many as seven doses of polio vaccine droplets over a period of months - a monumental logistics feat for poor countries, particularly in rural areas.
After years of struggle, India succeeded in vanquishing polio only when it switched its vaccine strategy to radically decrease the need for boosters. Instead of using an oral formulation that counters all three strains of polio viruses at the same time - but weakly - in 2009, India introduced a stronger vaccine that targets only the dominant two polio strains. The new vaccine gave children a 30 percent more powerful initial immune response, meaning that even without boosters, many Indian kids were protected. The impact was immediately felt, even in the poorest parts of the country. But this strategy may have rendered the children only temporarily protected, accounting for India’s fears of Pakistani vaccination failure.
Yet the government should also be concerned about its own population’s anti-vaccine movement, which has has reached middle-class India, where some parents decline immunization under false grounds that it would contribute to autism. The world is very close to victory, but the remaining challenges are more cultural and political than scientific.
Last year, a team of experts was deployed by the U.S. Agency for International Development to Afghanistan, Nigeria, and Pakistan to ask local villagers what the polio eradication effort was doing wrong. In village after village, they got the same astonishingly obvious answer: Stop sending teams of men to vaccinate our children.
Even a rudimentary understanding of conservative Muslim culture should have taught the would-be disease vanquishers that under Islam a woman may not allow an unrelated male into her home without her husband’s presence, nor should she allow the well-meaning gentleman to touch her female children. In all too many cases, vaccine failure boiled down to finally sending all-female health teams to Muslim-dominated villages. Though the WHO says the final eradication effort is shy $1 billion, money is less likely to decide the fate of the great polio elimination campaign than governance, politics, and culture in three hotbed nations. Which is why the CIA’s use of a phony vaccine campaign is so infuriating to health officials. It undermined the faith that many Muslims in vulnerable countries place in Western-inspired immunization and medicine. And with millions of children in India and some other countries now experiencing waning immunity, time is decidedly against us. If wild polio hasn’t been eliminated from the final three countries by the end of 2012, the virus could well resurge in sites of alleged eradication, all over the world. And thousands will suffer.
Laurie Garrett is senior fellow for global health at the Council on Foreign Relations and a Pulitzer Prize winning science writer.










