Every year, each one of us probably faces their share of colds, sore throats and viruses and when the symptoms are extreme, we try to find a way or a medium to get rid of it at as soon as we can by using antibiotics.
The misuse and overuse of antibiotics present a significant factor in the overall development of antimicrobial resistance and is recognised as one of the most serious health issues worldwide. Antibiotics, first used in the 1940s, are certainly one of the great advances in medicine. But overprescribing them has resulted in the development of resistant bacteria, that don’t respond to antibiotics that may have worked in the past. Across the region, multi-drug resistant bacteria are an increasing concern. Several bugs have become dangerously resistant to common antibiotics, making it harder for us to contain infections after even routine operations.
Doctors in the UAE suggest that overuse of antibiotics can make bacteria resistant to them and contribute to the evolution of “superbugs”. They call for implementing stringent regulations on over-the-counter antibiotic sales and in raising consumer awareness to reduce patient demand for antibiotics. Antibiotic resistance is of course not attributed to this alone.
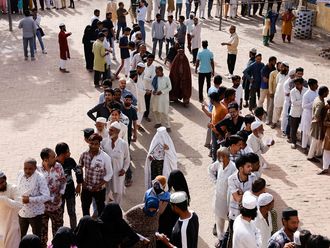
Researchers also suggest that poor hand-hygiene compliance has contributed to the spread of antibiotic-resistant bacteria. For example, it is due to this reason that health authorities recommend that those travelling to Saudi Arabia for the Haj, where millions of people from around the world congregate, should consult their physician beforehand to check their health and reduce risks of infection, rather than having to be treated with antibiotics later.
Implementation of basic hygienic routines is still largely absent in many hospitals and health-care settings worldwide. Cultural barriers and other challenges to their implementation need a deeper study. Infection-control interventions need to be reassessed and improved in an era with rapid transmission of multidrug-resistant bacteria and mobile antibiotic resistance genes.
Clinicians are advised to use antibiotics sparingly because their use kills off only the resistant types of bacteria, leaving non-resistant forms to multiply and become more prevalent, eventually making the antibiotics ineffective. Generally, efforts to improve microbiological laboratories are underway. Speed of testing and laboratory automation are crucial and have been the focus of recent developments.
Health-care professionals need to ensure they keep accurate, timely and clear medical records. Inaccuracies or improper record keeping may have devastating consequences for patients and all concerned.
Integrating all steps
In order to slow the emergence and prevent the spread of resistant bacteria and strengthen national and international efforts to identify and report cases of antibiotic resistance, we need to find adequate technology backing, e.g. a solution that automates and integrates all steps in the microbiology laboratory to improve productivity, streamline workflow and provide accurate results for the clinician to deliver better patient care — can help practitioners focus better and save valuable time and resources.
It is not just technology, but the entire system that needs to have processes in place, tools, education and programmes designed to increase staff competency, efficiency and overall productivity.
Superbugs are a significant health threat to societies at large. Proper detection is more important than ever, not only for patient care, but also for controlling the infection. Rapid identification and differentiation of these resistant bacteria are the keys to optimising treatment decisions that can significantly impact patient outcomes and cost of care.
To that extent, technology plays an important component in meeting laboratory testing needs. Reliable technology can allow microbiologists to control the overall growth of bacteria, while detecting any emerging resistance by providing accurate results in a timely and efficient manner.
Good communication encourages collaboration and helps prevent errors. It is important for health care organisations to assess possible setups for poor communication and be diligent about offering programmes and outlets to help foster team collaboration. By addressing this issue, health-care organisations have an opportunity to greatly enhance their clinical outcomes.
Dr Suleiman Al Obeid is MD, PhD, consultant clinical microbiology, head of the Microbiology Division, at the security forces hospital in Riyadh, Saudi Arabia.