London: In mid-June last year, Ali Mohammad Zaki, a virologist at the Dr Soliman Fakeeh Hospital in Jeddah, Saudi Arabia, took a call from a doctor who was worried about a patient.
The 60-year-old man had been admitted to the hospital with severe viral pneumonia and the doctor wanted Zaki to identify the virus. Zaki obtained sputum from the patient and set to work. He ran the usual lab tests. One after another they came back negative.
Puzzled by the results, Zaki sent a sample to a leading virology lab at the Erasmus Medical Centre in Rotterdam. While he waited for the Dutch team to examine the virus, Zaki tried one more test of his own.
This time he got a positive result. It showed the infectious agent belonged to a family of pathogens called coronaviruses. The common cold is caused by a coronavirus. So is the far more deadly infection Sars. Zaki quickly emailed the Dutch lab to raise the alarm. Their tests confirmed his fears, but went further: This was a coronavirus no one had seen before.
To alert other scientists, Zaki posted a note on proMED, an internet reporting system designed to rapidly share details of infectious diseases and outbreaks with researchers and public health agencies.
“This is a serious virus,” Zaki says.
Just how serious was clear. While Zaki had worked to identify the virus, the patient’s health had declined. His pneumonia worsened; his breath got shorter. His kidneys and other organs began to falter and fail. Despite all the drugs and dialysis, and mechanical ventilation to help him breathe, the man was dead 11 days after he arrived at the hospital.
On its own, the Jeddah case was more intriguing than terrifying. Though much was made of the virus being related to the one that causes Sars, which spread to more than 30 countries and killed 800 people in 2003, the two are genetically very different. Sars was scary because it spread so easily and killed so often. It circulated in families and tore through hospitals. The Jeddah patient was but a single case.
Or so it seemed. Since the virus came to light in September last year, the number of cases has risen to 33. More than half have died. On Sunday, the Saudi health ministry reported, two more people had died bringing the toll in the kingdom to nine, of 15 cases confirmed in total, Deputy Health Minister Ziyad Memish said.
The numbers are not yet alarming, but the steady appearance of fresh cases, and the fact that the infection has now spread from person to person, has sparked an intensive effort to understand the virus, and quietly prepare for the worst.
“We don’t know whether this virus has the capability to trigger a full epidemic,” says Ron Fouchier, a molecular virologist at Erasmus Medical Centre whose lab identified Zaki’s virus. “We are completely in the dark about it. We think what we are seeing is just the tip of the iceberg, but we don’t know how big the iceberg is, or where the iceberg is.”
Across from the Houses of Parliament on the bank of the river Thames is St Thomas’s Hospital, London. In September last year, doctors at the intensive care unit were struggling to diagnose a 49-year-old man from Doha, Qatar, who had arrived by air ambulance with a serious respiratory infection.
He was being treated in strict isolation. The man had a virus, that much was clear, but the nature of the infection was a mystery. He had recently visited Saudi Arabia.
Stumped by the case, doctors at the hospital alerted the Health Protection Agency’s (HPA) Imported Fever Service, which began its own investigation. Scientists ran tests on the Qatari man to exclude common infections. They then had a stroke of luck. The night they completed the first round of tests, two scientists on the HPA team logged on to proMED at home. There on the screen was a note published earlier that day from a Professor Zaki at a hospital in Saudi Arabia. It announced the discovery of a new and deadly coronavirus. The patient had almost identical symptoms to the Qatari man.
The next day, a Friday, the HPA ran fresh tests. The results were ominous. Tests for specific and well-known coronaviruses came up negative. But a general test for the coronavirus family was positive. That strongly suggested they were dealing with the same bug that had killed the man in Jeddah.
The HPA’s investigation switched up a gear. By late that Saturday, they had examined the virus’ genetic make-up and compared it with results Fouchier’s team had worked up on the Saudi virus. The viruses were 99.5 per cent identical. The HPA immediately told the World Health Organisation, which issued a global alert on the Sunday night.
But more cropped up elsewhere in the region. A Doha man fell ill and was transferred to a specialist lung hospital in Essen, Germany. He recovered and was discharged a month later. Back in Saudi Arabia, the virus struck a household in Riyadh, where a man lived with his two sons. One of the younger men died.
More worrying still was a cluster of cases in Jordan. In April 2012, 11 people, including eight healthcare workers, went down with a mystery respiratory illness. Posthumous tests on two who died were positive for the new virus. The others probably had the same infection, albeit more mildly, but follow-up tests were never done.
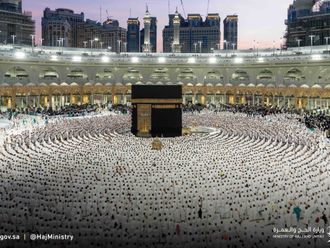
British health officials reported the first infection in a UK resident. The man, Abid Hussain, who is in intensive care in Manchester, fell ill on a trip to the Middle East. He flew to Pakistan to visit family, but stopped in Mecca on the way home to pray for his son, Khalid, who was being treated for brain cancer.
Soon after Abid arrived home, his son, who was on drugs to suppress his immune system, picked up the virus and died days later at Queen Elizabeth Hospital in Birmingham. Abid’s sister caught the virus too, but quickly recovered.
Khalid leaves a wife, Azima, and twin boys, who will be three this week. “They keep asking, ‘Where’s daddy? When is dad coming home?’, but they’re too young to know what’s going on,” Azima told the Guardian newspaper. The cluster of infections in the family has convinced scientists that the virus spread from person to person, albeit rarely.
There are no signs that the virus spreads easily from person to person. The HPA followed up 60-odd people, including doctors and nurses, who came into contact with the patient at St Thomas’s Hospital. They traced more than 100 others who had contact with the British family. None tested positive for the virus.
So far, so reassuring. But the virus will mutate and may adapt to spread more easily, scientists warn. “That is what we are worried about,” says Eric Snijder, head of molecular virology at Leiden University. “If that happened you might get a pandemic variant that spreads easily, and that would be a major problem.”